Connect With Us
Blogs
The Possible Causes of Feet Discoloration
Skin on the feet or ankles can discolor for any number of reasons, ranging from staining from wet clothes or boots to serious medical conditions. Yet, if the discoloration isn’t immediately explainable by simple environmental factors, then it’s in your best interest to seek medical attention.
Here are some things that you should know about some of the more serious problems that could be causing your feet discoloration.
Venous Insufficiency
Venous insufficiency, also known as chronic venous insufficiency or chronic venous stasis, is a problem with the flow of blood from the veins of the legs back to the heart. This occurs when the valves in the veins of the leg don’t work properly, causing fluid pools to form, which can lead to other problems including varicose veins.
Venous insufficiency can be caused by blood clots, deep vein thrombosis, or high blood pressure inside the leg veins. You are more likely to have venous insufficiency if you:
- Are older
- Are female
- Are overweight
- Don’t get enough exercise and tend to lead a sedentary lifestyle
- Smoke
- Have a family history of varicose veins
Symptoms may include:
- Swelling, often in the ankles
- Varicose veins
- Itching
- Cramping
- General weakness
- Skin sores (ulcers)
- Aching or a feeling of heaviness
- Changes in skin color/feet discoloration
- Thickening of the skin on your legs or ankles
In order to treat venous insufficiency, your doctor may ask you to:
- Wear compression stockings
- Get more exercise (especially walking)
- Avoid standing or sitting for long periods of time
- Keep your legs elevated when lying down
In more severe cases, you may have to undergo surgery to correct venous insufficiency. Your doctor may suggest one of the following types of surgery:
- Surgical repair of veins or valves
- Removing (stripping) the damaged vein
- Minimally invasive endoscopic surgery—the surgeon inserts a thin tube with a camera on it to help see and tie off varicose veins
- Vein bypass—a healthy vein is transplanted from somewhere else in your body (this procedure is generally used when the upper thigh is affected and only for very severe cases after nothing else has worked)
- Laser surgery—uses lasers to either fade or close the damaged vein(s) with strong surges of light in a small, specific place. It involves no surgical cuts.
Rocky Mountain Spotted Fever
Rocky Mountain spotted fever is a bacterial infection transmitted by a tick. Without prompt treatment, Rocky Mountain spotted fever can cause serious damage to internal organs, such as your kidneys and heart.
Although many people become ill within the first week after infection, signs and symptoms may not appear for up to 14 days. Symptoms can include:
- High fever
- Chills
- Severe headache
- Muscle aches
- Nausea and vomiting
- Restlessness and insomnia
- Rash—the red, non-itchy rash typically appears a few days after the initial signs and symptoms begin. It first appears on your wrists and ankles, and can spread in both directions.
People who develop Rocky Mountain spotted fever are much more likely to avoid complications if treated within five days of developing symptoms.
Ankle Sprain
An ankle sprain is an injury to the tough bands of tissue (ligaments) that surround and connect the bones of the leg to the foot. The injury typically occurs when you accidentally twist or turn your ankle in an awkward way. This can stretch or tear the ligaments that hold your ankle bones and joints together.
Symptoms of an ankle sprain can include:
- Swelling
- Bruising
- Pain
- Inability to put weight on the affected ankle
- Skin discoloration – primarily ankle and foot discoloration
- Stiffness
Treating a sprained ankle is important to promote recovery and to prevent further discomfort. If your sprain is mild, you should be able to treat it at home by:
- Using elastic bandages to wrap your ankle
- Wearing a brace to support your ankle
- Using crutches
- Elevating your foot with pillows while resting or sleeping to help reduce swelling
- Taking ibuprofen (Advil) or acetaminophen (Tylenol) to manage swelling and pain
- Getting plenty of rest and not putting weight on your ankle
- Applying ice every 20-30 minutes, three to four times per day
Surgery for ankle sprains is rare, but it may be performed when the damage to the ligaments is severe or when the injury doesn’t improve with non-surgical treatment. Surgical options include:
- Arthroscopy—your doctor will look inside the joint to see if there are any loose fragments of bone or cartilage
- Reconstruction—you doctor will repair the torn ligament with stitches. They may also use other ligaments or tendons around the foot or ankle to repair the damaged ligaments.
Proper Diagnosis
If you’re experiencing any feet discoloration, and the cause is not immediately known to you, you should seek out medical attention. A proper diagnosis can go a long way to helping you treat and quickly recover from whatever is causing your foot discoloration.
If you have any questions or concerns about feet discoloration, book an appointment with Dr. Vikki and Dr. Connie, so that they can help you get the right answers and treatment.
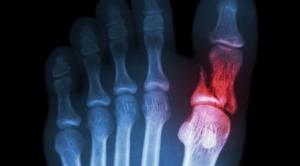
Here’s What Happens When you Don’t Treat a Broken Toe
You may have heard one of the many myths surrounding broken toes: that it will heal on its own, or that it’s okay as long as you can still walk on it. While reassuring, these common misconceptions are entirely false, and can have potentially severe consequences. Leaving a broken toe untreated can result in various complications, from misaligned bones and infection to arthritis and permanent foot pain. The thought of a doctor visit or hospital bill may make you cringe at first, but your feet will thank you for it in the long run.
Here is a look at the signs that your toe is broken, the dangers of avoiding treatment, and the steps you need to take to make sure your toe heals properly.
Signs Your Toe Is Broken
Even the smallest of accidents can result in toe trauma: dropping an object on the foot or stubbing your toe are common misfortunes that often lead to injury. Moreover, repetitive trauma to the toe over time can result in a stress fracture. While it’s tempting to try to tough it out, it’s important to listen to your pain to identify whether or not your toe is fractured.
It usually requires significant force to break a bone, although a little less so for the toes since their bones are so small. Regardless, the instance of fracture will be extremely painful. The toe will begin to swell as the fractured bone bleeds, resulting in bruising as the blood reaches the skin. You may also see blood pool beneath the toenail. In many cases an injury to the toe also involves damage to the toenail, which further increases your risk of infection should the toenail expose the tissue underneath. The fracture usually makes it extremely painful to walk, although this is not always the case. Even if you can still manage to walk on the toe, that doesn’t eliminate the possibility of a fracture.
Seek prompt medical attention if your toe shows signs of:
- Swelling
- Pain
- Bruising, or blue or gray spots surrounding the site of trauma
- Stiffness
- Trouble Walking
- Deformity
- Infection
- Bleeding, especially beneath the toenail
- Coldness, numbness, or a tingling sensation indicative of nerve damage
Complications of an Untreated Broken Toe
Leaving a broken toe untreated can have serious and long term complications, including, but not limited to:
- Infection: If the injury has left an open wound, or especially if there is damage to the toenail, you are at risk of contracting an infection. Any exposure of a broken bone can lead to a bone infection (osteomyelitis), which is usually caused by the bacteria staphylococcus aureus. Once diagnosed, your doctor may implement antibiotics straight into the bloodstream intravenously, or you may need to take medication for up to six weeks. If the infection is severe, your doctor may have to perform surgery to remove the infected bone.
- Compound fracture: A compound fracture is when a broken bone penetrates the skin, leaving the bone vulnerable to infection.
- Deformity: An untreated broken toe has a high likelihood of healing incompletely or improperly, potentially resulting in crookedness or deformity which may require corrective surgery down the road.
- Osteoarthritis: An improperly healed fracture can lead to a future of osteoarthritis as you age, generalized foot pain and discomfort, as well as an increased likelihood of further foot injury.
Toe Fracture Diagnosis and Treatment
Your podiatrist will order an X-ray to confirm a toe fracture. Once properly diagnosed, a mild toe fracture can be treated at home under the guidance of your trusted podiatrist. Home treatment essentials include elevating the foot above the level of the heart in order to decrease swelling, icing the injury for 20 minutes every 2 hours for the first 2 days, and of course rest and crutches to avoid bearing weight on the injury while you recover. OTC acetaminophen or ibuprofen should be sufficient for coping with the pain, although your doctor may prescribe a stronger medication if your fracture is severe.
If the fracture is minor or located in one of the small toes, your doctor may simply implement buddy taping, which involves taping the damaged toe to its neighbor for support while it heals. In cases where the toe fracture becomes rotated or displaced, the doctor will need to perform a reduction. This involves administering a shot of local anesthesia before realigning the toe back into its proper position.
Casting may be required in more severe fractures: where the big toe is injured, the joint is damaged, the injury involves various small toe fractures at once, or if a bone in the foot is injured in addition to the fractured toe. When wearing a cast, a sturdy shoe should be worn to provide maximum comfort and support. If all goes well, the fracture should take up to six weeks to heal.
Schedule a Consultation with Dr. Vikki and Dr. Connie
If you have suffered injury to your feet, toes, or ankles, don’t wait for complications to arise.Schedule a consultation with trusted podiatrists Dr. Vikki and Dr. Connie at the Superior Foot & Ankle Care Center today.
How to Bandage and Injured Foot
Whether you’re trying to help out a friend or you’ve hurt your own foot, knowing how to properly deal with and take care of an injured foot can save you a lot of stress and problems later.
Here’s a quick how-to guide on how to properly take care of and bandage an injured foot or ankle.
How to Stop Any Bleeding
If there is any blood involved, it is important to first wash your hands and put on medical gloves (if available) before applying direct pressure to the wound. If gloves aren’t available, use many layers of clean cloth, plastic bags, or the cleanest fabric available between your hands and the wound.
In order to stop the bleeding, you should:
- Have the injured person lie down and elevate their foot for a full 15 minutes
- Remove any visible objects in the wound that are easy to remove
- Remove clothing and jewelry from the general area of the wound in case of swelling
- If blood soaks through the cloth, apply a clean one
How to Wrap an Injured Foot or Ankle
To prevent further injury and encourage proper healing, you should make sure that you protect and compress your foot, as well as rest, ice, and elevate your injury. There are a couple different types of material that you can use to wrap and compress an injured foot or ankle, including an elastic cloth bandage and athletic tape.
Wrapping with an Elastic Cloth Bandage
- Begin wrapping—place the end of the bandage where the toes meet the foot. Begin by wrapping the bandage around the ball of the foot. Hold the end of the bandage against the ball of the foot with one hand, and use the other to bring the tail around the foot from the outside. Make sure to keep the bandage tight, but not so tight that it decreases blood flow to the foot and toes.
- Work your way toward the ankle—wrap the ball of the foot twice, to hold the bandage in place, then begin moving up towards the ankle, being sure to leave at least one-half inch of bandage overlapping the previous layer. Make sure the layers are smooth and even with no unnecessary bulges or lumps. Start over if you need to do the job more neatly.
- Wrap the ankle—when you get to the ankle, bring the end of the bandage up outside of the foot, over the instep and around the inside of the ankle. Then bring it around the heel, back up over the instep, under the foot and around the ankle. Continue making a figure eight around the ankle several times to fully stabilize the ankle.
- Finish the wrap—the last wrap should rise several inches above the ankle to help stabilize it. Use the metal fasteners or medical tape to secure the remaining bandage. Excess bandage can also be tucked under the last layer, provided there’s not too much excess.
Wrapping with Athletic Tape
- Decide if athletic tape is right for you—while athletic tape works to wrap an injured ankle, it is primarily made to wrap an uninjured joint before physical activities to avoid injury, not to protect an already injured ankle.
- Begin with an underwrap—underwrap is a non-adhesive material used to wrap the foot and ankle before tape is applied, so that the tape doesn’t pull at the surface of the skin. Starting at the ball of the foot, wind the underwrap around the foot up to the ankle, leaving the heel uncovered.
- Secure the anchor—cut the strip of tape long enough to wrap one and a half times around your ankle. Wind it around your ankle, over the underwrap, to hold the underwrap in place.
- Create a stirrup—place the end of a piece of tape on one side of the anchor. Bring it down under the arch of the foot and back up to the other side of the anchor. Press it lightly to secure it in place. Repeat with two more pieces of tape overlapping the first one to create a sturdy stirrup.
- Create an X over the foot—place the end of a piece of tape at the ankle bone and run it diagonally over the top of the foot. Bring it down under the arch and toward the inside of the heel. Then bring it around the back of the heel and back up over the foot to create the other part of the X.
- Make a figure eight—place the end of a piece of tape on the outside of the ankle, just above the bone. Run it over the top of the foot at an angle, then bring it under the arch and up the other side of the foot. Next bring it around the ankle and back to the point where you started. Use another piece of tape to make a second figure eight that overlaps the first one. This will ensure that the wrap is held securely in place an provides enough support for the ankle to heal properly.
If a foot or ankle injury is serious and/or life-threatening, it’s important to call an ambulance. However, if the pain is manageable and you need help in dealing with the injury and getting back on your feet as soon as possible, be sure to get in contact with Dr. Vikki and Dr. Connie today.
Potential Causes of Itchy Feet
Itchy feet can become the bane of any day: you’re either driven mad trying to resist the urge to scratch; or by the redness, swelling, cracking, and flaking as a result of uncontrollable itching. While the cause could be something benign such as dry skin or excessive sweating, it could also indicate an infection or undiagnosed skin condition. Moreover, if left untreated, other complications could arise, such as a secondary infection.
The itching and burning will only continue to plague you until you accurately identify the source and treat it accordingly. Besides the obvious bug bites or allergic irritation, itchy feet are most commonly caused by a fungal infection or an underlying skin condition. In rare cases, itching could also suggest the presence of another medical condition, such as diabetes. Only examination from a trusted podiatrist can accurately diagnose your foot condition.
Here’s a look at the possible causes of itchy feet, treatment, and prevention tips to keep your feet feeling fresh.
Fungal Infection
When itchy feet are the main symptom, fungal infection is usually the primary suspect: specifically, tinea pedis, or athlete’s foot. Constant exposure to sweat and bacteria, in addition to walking barefoot on contaminated surfaces, make your feet the ideal breeding ground for fungal infection.
Athlete’s foot is an extremely contagious fungal infection which is easily spread through contact with infected surfaces, usually in damp spaces such as showers and gym locker rooms. In fact, it can even be spread through shared towels or linens. The first sign of infection is a dry, scaly rash that causes unbearable itching on the bottoms of the feet and between the toes. While the symptoms can be abated by certain over-the-counter creams, only a podiatrist can effectively cure you of the infection. Once cured, vigilant prevention should be practiced to avoid re-infection.
Skin Conditions
A number of skin conditions can lead to insatiable itching of the feet.
Eczema: Eczema can affect most parts of the body, but dyshidrotic eczema specifically affects the feet and hands. It is characterized by tiny itchy blisters formed on the soles of the feet, which then dry and cause cracking on the skin. If not properly cared for, the exposed skin can become vulnerable to infection. Since dyshidrotic eczema can share symptoms with other skin conditions, a skin sample will likely be taken for proper diagnosis.
Contact dermatitis: Contact dermatitis is a skin irritation that results from contact with an allergen or irritant, which appears similar to a rash. Allergic contact dermatitis is caused by skin exposure to an allergen, triggering an allergic reaction in the affected area. Irritant contact dermatitis is distinct in that it does not involve the immune system, but is instead the result of skin damage caused by exposure to an irritant that rids your skin of its protective surface oils. Common triggers of contact dermatitis include poison ivy, latex, nickel, chemical fragrances, topical medications, and leather.
Psoriasis: Psoriasis is an autoimmune disorder which causes rapid skin cell turnover, resulting in incredibly itchy and scaly dry patches called plaques. The plaques are the result of layers of new skin cells rising so quickly that the dead skin piles atop the surface, rather than gradually sloughing off, form dry patches of thickened skin. Plaques are commonly found on the bottoms of the feet, as well as the elbows and knees.
Additional Sources of Itchy Feet
Here are a few potential, albeit less likely, perpetrators of itchy feet:
- Diabetes: Skin conditions can sometimes indicate diabetes. A condition called eruptive xanthomatosis produces small itchy bumps on the skin as a result of severe diabetes. The condition subsides once the diabetes is managed and under control.
- Scabies: Scabies is an infection of the human itch mite which burrows just below the skin to lay its eggs. The infestation causes intense itching which worsens at night, a pimply rash, and tiny blisters. You can also see traces of the burrows on the skin, which appear as thin whitish lines along the surface. Scabies is easily spread, and should receive medical attention to stem the infection right away.
- Pitted Keratolysis: Pitted keratolysis is a non-contagious bacterial infection, caused by wearing damp, restrictive footwear. It produces shallow pits beneath the toes and soles of the feet, accompanied by itching, burning, and an extremely foul odor.
Prevention Tips
The feet are constantly plagued by bacteria, and need to be cleaned just like your hands. To keep your feet comfortable and fresh, follow these basic hygiene tips:
- Avoid walking barefoot anywhere, especially on damp communal surfaces.
- Always wear dry, clean socks and shoes made of breathable materials.
- Wash your feet thoroughly, and do your best to keep them dry.
- If someone you know has an infection, do not share towels or linens, and protect your feet from contaminated surfaces.
- Keep your toenails trimmed and clean.
If you suspect an infection is already present, schedule an examination with a reputable podiatrist right away.
Schedule a Consultation with Dr. Vikki and Dr. Connie
If itchy feet are wreaking havoc on your life, schedule a consultation with esteemed podiatrists Dr. Vikki and Dr. Connie at the Superior Foot & Ankle Care Center today.
Professions That can Exacerbate Foot Problems
There are some professions out there that cause a lot of stress to the arches, balls and heels of the feet, which can lead to other spinal and back discomfort issues, fatigue, and various mental health problems. Health care professionals, construction, hairdressing, office jobs, as well as landscaping jobs are all very different professions with this commonality—all are very stressful for the feet and can cause foot problems and pain.
Health Care Professionals
Hospitals are one of the busiest public places where employees work long hours. Nurses and doctors are always on the move during their long shifts, walking miles each day to serve and assist their patients. This can lead to numerous foot problems such as bunions, flat feet, ingrown nails, and heel spurs.
The foot has dozens of bones, joints, muscles, nerves, blood vessels, tendons, and layers of connective tissue. When working in the health care profession and working those long hours on your feet, the body tissues in your feet can become very stressed, achy, and swollen. If there is prolonged inflammation, this will actually form scar tissue and tire out the bones of the feet.
For those that work in the healthcare profession, be sure to wear comfortable, arch-supportive shoes with shock-absorbing soles, and get them fitted by a professional to make sure they are exactly right for your feet.
Construction Workers
Construction work is a heavy-duty, active profession that puts a lot of strain on the entire body, including the feet. Construction workers have to work in very challenging weather and circumstances and are on their feet for their entire day besides some small breaks. They are required to bend and lift and tend to end their shifts very exhausted and, sometimes, in pain.
The most common injury experienced by construction workers are ankle and foot injuries. Construction workers often develop flat feet or severely painful arch problems that can hinder their performance and their lifestyle outside of work.
Construction workers should invest in good footwear, such as steel-toe boots, that are a high quality brand able to prevent blisters, calluses, and protect the feet from anything heavy that could fall on them. Weeks before working in new boots, it’s key to break them in as much as possible.
If construction workers experience a foot injury, they should take days off to recover and see a medical professional like a podiatrist who can identify the problem and prevent further pain and injury.
A great tip is to freeze a bottle of water before heading out to work. When you get home, roll your feet over the frozen bottle. Not only will this exercise reduce inflammation and pain, but also the motion of the rolling will get the blood moving in your feet.
Hairdressing
Hairdressers often complain of foot pain at work, and this can result from repetitive straining motions; but also from a lack of supporting your feet and preventing foot problems well before pain and problems occur. If you are a hairdresser, try to remember to not lean on one dominant side when cutting hair.
Try to ground yourself and distribute your weight evenly on both of your feet. This will prevent pinched nerves and developing uneven arches.
Another way to prevent foot problems is to exercise and have a balanced diet. The more weight you carry, the more strain that’s placed on your feet, legs, and back. It’s simple—the more you weigh, the harder it is for you to be standing on your feet day all day.
Invest in a rubber mat for your chair and work space area. This will prevent developing foot problems and will keep your back healthy, too. Wear good shoes with less than a 1.5-inch heel to avoid severe heel pain. Absorbent pads and laces on the body of the shoe can help provide optimal support. Consider orthotics if you’re already experiencing foot pain as this will alleviate and correct current problems.
Preventing Foot Problems
Healthy feet are the key to a healthy life. Talk to a podiatrist professional such as the great team at the Superior Foot and Ankle Care Center and learn more about what you can do to keep your feet healthy.
What Could be Causing Your Child’s Pigeon Toe?
Have you ever noticed that your child walks with their feet turned inward? Does this worry you? It is possible that your child has pigeon toe. But before you start stressing out with worry, here are some things that you need to know about pigeon toe and what might be causing the problem.
What is Pigeon Toe?
Pigeon toe (also known as in-toeing, false clubfoot, in-toe gait, metatarsus adductus, or metatarsus varus) is a condition that causes the toes to point inward. This condition is common in infants and young children. If your child is pigeon toed, it doesn’t mean that there’s something wrong with their feet, and it is not necessarily a problem. The term merely refers to the way the toes point when walking.
Pigeon toe isn’t painful of bothersome, nor is it known to cause other medical problems such as arthritis. Some of the symptoms of pigeon toe are:
- Feet pointed inward (as if the toes are touching)
- Stumbling (severe cases)
- Clumsiness
Causes of Pigeon Toe
Pigeon toe can have a few different causes that are normal variations in the way the legs and feet line up. The three conditions that can cause pigeon toe are: metatarsus adductus, tibial torsion, and femoral anteversion.
Metatarsus Adductus
This occurs when the foot tends to resemble a kidney, or when the metatarsus adductus has an inward curve at the outer edge of the foot.
If your child has this condition, you will probably notice it while they’re still a baby. Sometimes your doctor might try braces or special shoes while the child is still a baby (six to nine months old) to help the bones grow straight.
This condition will not clear up on its own. It requires treatment which will vary depending on whether the condition is flexible or fixed. Most flexible cases respond well to passive stretching, bracing, or specialized shoes, where as fixed types require serial plaster casting (casts on the feet and lower legs that are usually put on before the child is eight months of age).
If the treatment for flexible cases doesn’t work, then your child will be re-evaluated to make sure that they don’t have club-foot instead of metatarsus adductus. Surgical correction may be necessary, especially in cases of club-foot.
Tibial Torsion
This occurs when there is an inward twist of the tibia (shin) bone. This is commonly seen in children learning to walk (under two years of age).
Even with the twisted shin bone, the knees will still point straight ahead. This condition may be a result of the baby’s position in the mother’s womb before being born.
Usually the leg will straighten out within the first year of life as the baby starts pulling up and standing, but some children may continue to walk pigeon-toed until the leg bone is done growing. Surgery may be necessary for children who don’t outgrow this condition by the age of 10.
Femoral Anteversion
This occurs when there is an inward twist at the upper thighbone. The kneecap tends to point inward when the child is walking.
Most children show this form of pigeon toe between the ages of two and four, after they have begun walking. Children with a twisted thigh bone often sit with their legs crossed, and the best way to treat this condition is to have them sit in a chair with their legs uncrossed. This condition usually clears up by itself, but it may take one to three years for the thigh bone to straighten. Generally, a child will outgrow this condition by age eight.
Treating Pigeon Toe with Exercise
While pigeon toe usually corrects itself as the hip bones strengthen, there is a chance that, in some young children, the hip bones may remain weak or the shin bones of the lower legs might turn in. Treatments for this may include physiotherapy, with exercises such as:
- Have your toddler or young child sit up straight in a child-size firm chair. Help your child sit in the chair with their legs uncrossed and feet flat on the floor. Trace your child’s feet in the correct slightly outward position onto a piece of paper and have your child sit in the chair with their feet in the outlines. Continue this exercise daily until the condition is corrected.
- Teach your toddler or young child to walk backward. Clear an area of about six square feet in your living room or backyard to avoid injuries. Continue this exercise for up to 10 to 20 minutes or as long as your child is able to do so. This exercise will help strengthen your child’s hip joints. Repeat this exercise regularly during play and walking time.
- Make a low walking beam for your child to walk on. Place the board of wood on two square pieces of wood or two bricks. Keep the plank three to five inches off the ground to avoid injury due to falling. Help your child walk across the plank two to four times a day and continue this exercise regularly until their walking is normal. This exercise helps the child place one foot in front of the other correctly, and strengthens the muscles that keep the hip and shin bones aligned.
Book a Consultation
Before you try to diagnosis your child’s pigeon toe on your own, you should make an appointment with a qualified podiatrist. Book a consultation with Dr. Vikki and Dr. Connie today so that they can help you figure out the right treatment plan for your child’s pigeon toe.
How to Minimize Foot Inflammation
Foot Inflammation is the body’s attempt to fend off foreign, invasive objects, including bacteria or viruses. In other words, inflammation is an immunological response to remove potentially harmful foreign stimuli and to heal the site of invasion.
Inflammation often begins with irritation, and is then followed by suppuration (pus discharge). Then there is the granulation stage – the formation in wounds of tiny, rounded masses of tissue during healing.
Symptoms of inflammation include redness, swelling, pain, localized stiffness, and loss of functions. These symptoms may not often be concurrently present. Inflammation may also cause flu-like symptoms including fever, chills, fatigue or lethargy, headache, loss of appetite, and muscle stiffness.
Common Causes of Foot Inflammation
Foot inflammation is caused by injury, overuse, or other conditions causing inflammation of the bones, ligaments, or tendons in the foot. A list of common causes for foot pain can include, but are not limited to, the following:
- Achilles tendinitis
- Arthritis
- Bone spurs
- Broken ankle/broken foot
- Bunions
- Corns and calluses
- Diabetic neuropathy
- Gout
- Hammertoe and mallet toe
- High heels or poor-fitting shoes
- Ingrown toenails
- Osteoarthritis
- Paget’s disease of bone
- Peripheral neuropathy
- Plantar fasciitis
- Plantar warts
- Stress fractures
Preventing Foot Inflammation
As necessary and inevitable as it is that we rely on our feet for mobility to engage in daily activities, there are many ways in which we can care for our feet so they continue to support us without causing us pain:
- Maintain a healthy weight: As the weight-bearer of the body, the more weight our feet have to support, the more stress they are put under. As little as 20 extra pounds on your body will change the way your feet function, increase the stress on your feet, and possibly trigger pain. If foot pain occurs during exercise, try switching to a low-impact sport such as swimming.
- Boost flexibility: Stretch the calf muscles on a regular basis, as they tend to tighten as you age, thus putting extra stress on your feet. Try the following calf-stretching exercise three times a day:
- Stand with your toes on a step with your heels of the edge.
- Slowly lower your heels and hold for 10 seconds; lift your heels to the starting position.
- Repeat five to 10 times.
- Do not force your heel farther than what feels comfortable. Complete the exercise one foot at a time if necessary.
- Avoiding high-heels: Wearing high-heels shortens calf-muscles and increases the likelihood of experiencing back pain. One study found that it takes only 66 minutes of wearing heels for the pain to kick in. Moreover, forcing your feet into pointy-toed heels can cause foot ailments such as ingrown toenails, bunions, blisters, and deformed toes.
- Ensure a comfortable fit: Feet change in shape in size as you age, so it is important to have your feet measured before you purchase a new pair of shoes. In addition, it is common to have feet of different size; therefore, be sure to have both feet measured and buy the size that fits the larger foot. Before purchase, also make sure there is about half an inch of wriggle room between your longest toe and the front of the shoe. Shop for shoes in the afternoon when your feet are usually at their largest, and wear the socks you would normally wear with the particular type of shoes.
- Take seated breaks: If you need to be on your feet most of the day, try to take seated breaks during which your feet can rejuvenate.
- Trim your toenails with care: Ingrown toenails are a common source of foot pain. Cut your toenails straight across; do not cut around the corners to match the shape of your toe.
- Stay hydrated: Dehydration can cause foot cramps, which can come on suddenly and cause sharp, debilitating pains. Drinking plenty of fluids, and eating food rich in potassium such as bananas and spinach will minimize the risk of experiencing foot cramps.
If you’ve taken the above steps and find that your foot inflammation is not alleviating itself, be sure to get in contact with Dr. Vikki and Dr. Connie today.
How you Can Improve Your Posture Through Your Feet
Do you find that you often have back or joint pain? Has anyone ever told you that you have terrible posture? The two are connected, and both have a lot to do with your feet.
Improper foot alignment can cause an array of problems, but you don’t have to live with them forever. Here are some quick tips on how to fix your posture by focusing on your feet.
How the Feet Work
Before you can learn how to fix your posture by focusing on your feet, it is important that you understand the feet themselves. Each foot has 26 bones, 33 joints, and more than 100 muscles, tendons, and ligaments. The foot is divided into three parts: the hind foot (the ankle bone and the heel bone), the mid foot (a group of five irregular bones in the arch of the foot), and the forefoot (the metatarsals and toes).
Our feet move in different ways:
- Plantar flexion of the ankle, which occurs when you stand on tiptoes. If you’re sitting with your legs out in front of you, plantar flexion of the ankle happens when you point your toes.
- Dorsiflexion, which occurs when you stand on your heels with the balls of your feet lifted off the floor. If you’re sitting, dorsiflexion happens when you push your heels away from you and pull your toes toward you.
- Supination, which takes place when you stand with your weight rolled onto the outer edges of your feet, lifting the arches and the base of the big toe. Non-weight bearing supination happens when you sit with your legs out in front of you and turn the soles of the feet so they start to face each other.
- Pronation, which happens when you lift the outer edges of your feet as you stand, collapsing your arches. In sitting postures, pronation occurs when you press out through your inner heels and the bases of your big toes.
Correct distribution of weight in your feet can help give your body optimal postural alignment.
Common Problems and How to Fix Them
Two of the most common foot problems that can affect your posture are pigeon toes and duck feet.
Pigeon Toes
Cause: Weak glutes (butt muscles) and overactive tensor fasciae latae (outside of your hip).
Fix: Lie on one side with your knees bent 90 degrees and your heels together. Keeping your hips still, raise your top knee upward, separating your knees like a clamshell. Pause for five seconds, then lower your knee to the starting position. That’s one rep. Perform two or three sets of 12 reps on each side daily.
Duck Feet
Cause: Weak oblique muscles and hip flexors, and overactive piriformis and the other deep external rotators (muscles really deep in your hip attaching the femur to your sacrum).
Fix: Get into a push-up position with your feet resting on a stability ball. Without rounding your lower back, tuck your knees under your torso, using your feet to roll the ball toward your body, then back to the starting position. That’s one rep. Do two or three sets of six to 12 reps daily.
Making Small Changes
While exercising your feet can definitely help with your overall posture, you should also consider making small changes to your everyday life. Some of the things that you can do include:
- Being aware—take a while to study how you stand, or have your doctor on your next visit look at your legs and their alignment. A yoga therapist, chiropractor, or podiatrist with an extensive background in anatomy and physiology can do this for you, as well.
- Make adjustments—your body might just need a change in how you walk. For example, if you notice you walk more toward your instep, adjust how you walk on your own. Find that correct distribution of weight and movement in your feet.
- Build muscle strength and relaxation—if you have fallen arches, those muscles might be weak, work on them with yoga poses specifically targeting those muscles in the lower legs. In turn, some muscles may be too strong, pulling your leg and pelvis in a certain direction. Work on relaxing those in addition to building strength in your weaker sections.
- Use traction exercises—traction, when done manually with a strap or belt, can be a great way to gently work your problem areas back to their most favorable shape, strength, or position.
- Walk barefoot—our feet were made to walk just as they are. Putting them in heels or tennis shoes brings the foot into an unnatural shape, no matter how much they are advertised to be good for walking, running, or any other activity.
- Try not to rely on insoles—you can have customized insoles for your shoes, and although they do make you feel better when you wear your shoes, they can’t always completely fix the problems that you’re having.
- Be kind—treat your feet with kindness. Remember to massage your feet to release tension. Using a hard rubber ball under the soles and moving the foot back and forth works wonders.
Treating Improper Posture with Dr. Vikki
Since fixing the way your feet take your weight can help correct your overall posture, it is important that you have your feet properly examined by an experienced podiatrist. Book an appointment with Dr. Vikki and Dr. Connie today, so that they can help you get your feet back on the right track.
What you Need to do When you Have a Foot Fracture
A foot fracture occurs when one or more of the 26 bones of the foot break as a result of either a sudden trauma or chronic overuse. In general, foot fractures come in two broad categories:
- Full foot fracture: typically a result of a one-time trauma to the foot, such as a car crash or impact from a blunt and heavy object to the foot.
- Stress fracture: caused by repeated stress to a bone or multiple bones in the foot, a stress fracture may sound less severe than a full foot fracture, but it still entails a breakage of the bone in the foot.
There are, in addition, different types of bone fractures depending on their nature:
- Non-displaced: when a bone breaks but stays in place.
- Displaced: when a bone breaks into two pieces that move apart from one another.
- Comminuted: when a bone is broken in multiple places in the foot.
- Open fracture: when a bone breaks through the skin after fracturing.
Home Treatment for a Foot Fracture
If you suspect that a fracture might have occurred, it is best to err on the side of caution and apply first aid treatment to the affected foot. The acronym RICE can help you remember what to do in such a situation:
Rest: Rest the affected area. Stay off the injured foot until it can be fully evaluated. Walking, running, or playing sports on an injured foot may exacerbate the injury.
Ice: Apply ice to the affected area as soon as possible, and reapply it for 15–20 minutes every three or four hours for the first 48 hours after injury. Ice helps decrease inflammation.
Compression: Wrap an elastic bandage around the affected foot. The wrapping should be snug, but not so tight as to cut off circulation.
Elevation: Elevate the affected extremity; ideally, your foot should be elevated higher than your chest/heart area. Keeping your foot elevated decreases blood flow to the area, and thus decreases swelling.
Using nonsteroidal anti-inflammatory drugs such as ibuprofen or naproxen can help relieve pain and reduce swelling.
Visiting a Podiatrist for a Foot Fracture
If you notice increased pain, swelling, bruising, redness, or difficulty walking after an injury, you should see a podiatrist immediately. A podiatrist will take a complete medical history while examining your foot to look for areas of tenderness by applying gentle pressure directly to the injured bone. Often, the key to diagnosing a stress fracture is the patient’s report of pain in response to this pressure.
The podiatrist may then order tests, including an X-ray, ultrasound, or MRI, to determine the extent of your injury. You may not need further testing beyond an X-ray if it clearly indicates the location of the fracture. Otherwise, ultrasounds and MRIs will be useful for finding soft issue injuries (including torn ligaments) and fractures that might not have shown in an X-ray.
Treatment Options for Foot Fractures
Treatment for a foot fracture will depend on your injury. If you have a broken bone, your podiatrist may attempt to reduce the fracture by lining up the ends of the bones so they can heal properly (reduction). You’ll be given a local anesthetic to numb the area should this be your treatment option.
An unstable fracture in which the ends of the bone do not stay in place after a reduction may require surgery. Internal fixation is the procedure during which pins, screws, and/or metal plates are used to hold the small bones of the foot together during the healing process.
Caring for a Fractured Foot
Your podiatrist may recommend that you use crutches to keep weight off your foot until the pain subsides. Other recommendations for caring for your injury during the healing process include:
Modified activities. It typically takes from 6 to 8 weeks for a stress fracture to heal. During that time, switch to activities that place less stress on your foot and leg. Swimming and cycling are good alternative activities; although you should not resume any type of physical activity that involves your injured foot or ankle – even if it is low impact – without your podiatrist’s recommendation.
Protective footwear. To reduce stress on your foot and leg, your podiatrist may recommend wearing protective footwear. This may be a stiff-soled shoe, a wooden-soled sandal, or a removable short-leg fracture brace shoe.
Casting. Stress fractures in some of the bones of the foot, such as the fifth metatarsal bone (on the outer side of the foot), take longer to heal. Your podiatrist may apply a cast to your foot to keep your bones in a fixed position and to remove the stress on your involved leg.
If you believe you’ve suffered a fracture anywhere in either of your feet, be sure to get in contact with Dr. Vikki and Dr. Connie at the Superior Foot and Ankle Care Center.
Conditions and Diseases That Cause Foot and Knee Pain
You may be surprised to learn that a lot of the problems you have with your feet might also be the cause of your knee pain. Here’s a quick look at some of the conditions and diseases that can cause a combination of foot and knee pain.
Flat Feet
Many people with flat feet find that their ankles roll inward with each step. This excessive inward rotation of the ankle, tendons, and ligaments connecting the muscles and bones of the heel and shin bone will cause the inside of the lower leg to stretch further than the outside. As the lower leg is pulled out of line, the knee fails to track straight, causing knee pain.
There are a few ways in which you can tell if you have flat feet:
- Get your feet wet and make an impression on a dry patch of flooring. The inside of the impression should be dry, as a healthy arch wouldn’t have made contact with the floor.
- Place the soles of your feet together. Check to see if each instep is virtually in contact along the length of your feet, or whether there is a good parting of the feet around the midsection.
- See if you can comfortably insert your thumb under your instep while standing.
Osteoarthritis
Osteoarthritis occurs when the protective cartilage one the ends of your bones wears down over time. With osteoarthritis, the slick surface of the cartilage becomes rough and may eventually wear down completely, causing bone to rub on bone. It can damage any joint in your body, including your feet and your knees.
The symptoms of osteoarthritis often develop slowly and worsen over time. Symptoms include:
- Pain
- Tenderness
- Stiffness
- Loss of flexibility
- Grating sensation
- Bone spurs (extra bits of bone that feel like hard lumps)
Rheumatoid Arthritis
Rheumatoid arthritis is a chronic inflammatory disorder that can affect more than just your joints. In some people, the condition can also damage a wide variety of the body’s systems, including the skin, eyes, lungs, heart, and blood vessels. Rheumatoid arthritis affects the lining of your joints, causing a painful swelling that can eventually result in bone erosion and joint deformity.
The condition occurs when your immune system attacks the synovium (the lining of the membranes that surround your joints). The resulting inflammation thickens the synovium, which can eventually destroy the cartilage and bone within the joint. The tendons and ligaments that hold the joint together weaken and stretch, gradually causing the joint to lose its shape and alignment.
Tendinitis
Tendinitis, or tendonitis, is an inflammation or irritation of a tendon (a thick cord that attaches the bone to muscle. It is most often caused by repetitive, minor impact on the affected area, or from a sudden more serious injury. Incorrect posture at work or home, or poor stretching or conditioning before exercise may increase your risk of tendinitis. Tendinitis can occur almost anywhere in the body where a tendon connects muscle to bone, and can affect anyone of any age.
Symptoms of tendinitis include:
- Pain at the site of the tendon and surrounding area
- Loss of motion
Bursitis
Bursitis in a painful condition that affects the small, fluid filled sacs (bursae) that cushion the bones, tendons, and muscles near your joints. Bursitis occurs when bursae become inflamed, and most often occurs in joints that perform frequent repetitive motion.
Symptoms of bursitis can cause the affected joint to:
- Feel achy or stiff
- Hurt more when you move or press on it
- Look swollen and red
Gout
Gout is characterized by sudden, severe attacks of pain, redness, and tenderness in the joints. It is a complex form of arthritis that can affect anyone, but is more common among men. Gout occurs when urate crystals accumulate in your joint, causing inflammation and intense pain. Urate crystals can form when you have high levels of uric acid in your blood. Your body produces uric acid when it breaks down purines (substances found naturally in your body), as well as steak, organ meats, and seafood.
Symptoms of gout include:
- Intense joint pain
- Lingering discomfort
- Inflammation and redness
- Limited range of motion
Treating Foot and Knee Pain
If you suspect that you have any of the above conditions or diseases, then you should schedule a consultation with Dr. Vikki and Dr. Connie. With years of collective experience in their fields, they have the experience to help you figure out what the root of your problem is.