Connect With Us
Blogs
Preventing Diabetic Foot Problems
Did you know that more than 60% of all non-traumatic lower limb amputations are the result of complications from diabetes? The good news, however, is that you can reduce your risk of amputation by up to 85% and of other diabetes related foot problems as well by partnering with you podiatrist. November is National Diabetes Month and we at Superior Foot & Ankle Care Center want to help you prevent foot health issues commonly associated with diabetes.
Detecting Trouble Early
Neuropathy or nerve damage frequently affects patients with diabetes. Lack of feeling in your feet make it difficult to perceive pain, temperature changes and other signs that typically let your body know there’s a problem. As a result, sores and ulcers, calluses, infections and skin problems can all develop to a fairly serious level before being detected by the patient. One of the best steps you can take to prevent diabetic foot issues is to check your feet daily (or have someone do for you) for injuries or changes. Here’s what to look for:
- Changes in skin color
- Temperature changes
- Swelling of your ankle or foot
- Bruises, sores, cuts or red spots
- Dry skin, cracks in the heel or skin
- Corns, calluses and blisters
- Toenail changes—including discoloration, thickening, becoming ingrown
Avoiding Foot Issues
There are a number of ways to prevent diabetic foot problems from developing:
Visit Your Podiatrist–Diabetic patients should have two regularly scheduled exams annually with one of our board certified foot and ankle surgeons, Dr. Victoria Foley and Dr. Constance Omelas to check the health of your feet. In addition, if you notice any of the changes listed above, you should make an appointment immediately.
Wear Properly Fitted Shoes–It’s essential that shoes have a roomy toe box and enough room to prevent cramping and also so that no rubbing or friction against the skin occurs.
Don’t go Barefoot–Even at home, the risk of cuts, injuries and infections are too great.
Exercise–A moderate exercise program (approved by your physician) will help improve blood flow to the feet as well as control blood sugar and weight—all key for managing diabetes.
If you have more questions on diabetic foot care, don’t hesitate to contact our Long Beach office at: 562-420-9800.
What’s Behind Tendonitis?
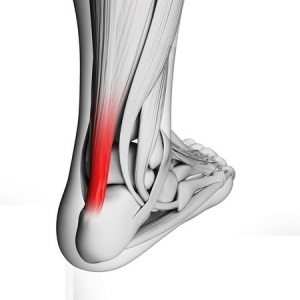
The day after a particularly intense workout or a long run you may notice pain ranging from mild to extreme in the lower part of the back of your leg. Or, you may be noticing a sluggish feeling in your leg accompanied by stiffness and/or a dull ache that lessens as you stretch the leg and get going with your day. All of these are possible symptoms of Achilles tendonitis—an inflammation of the large tendon that runs between the bottom of your calf muscle and your heel that we see often at Superior Foot & Ankle Center.
Tendonitis is primarily caused by overuse or trauma to the tendon. Scenarios that can result in inflammation and injury to the Achilles tendon include:
- Suddenly increasing the distance or intensity of your run or workout
- Doing too much too soon in a new exercise routine or starting up after a period of inactivity
- Overpronation
- Inappropriate footwear choices
- Not stretching enough before sports or exercise
- A trauma to the tendon caused by a sudden or wrenching movement (like taking off for a sprint)
- Heel bone deformity
- Age related wear and tear
Treatment and Prevention
Mild cases of Achilles tendonitis can be resolved by resting the leg and avoiding activities that put stress on the tendon. If the pain is persistent however, and doesn’t seem to improve with rest, it’s time for an appointment with one of our podiatrists, Dr. Victoria Foley or Dr. Constance Omelas. The foot doctor can evaluate just how severe the tendonitis is and make recommendations for relief. These may include: icing, specific stretching exercises to do before and after exercise and a heel cup or other orthotic device to help prevent overpronation and increase arch support. Wearing properly fitting shoes that are designed for the sport or activity you do and following a sound program that increases in intensity gradually can help prevent inflammation the Achilles tendon.
To learn more about how to prevent or treat Achilles tendonitis, call our Long Beach office at: (562) 420-9800.
Treating Sprained Ankles
Among the more common injuries we see at Superior Foot & Ankle Care Center are ankle sprains. In many instances these injuries come about on the playing field in soccer or football, for example, when your foot is planted and headed one way and then suddenly gets twisted in a different direction. Ankle sprains can also occur less dramatically, like stepping off a curb or missing the bottom step.
How Severe is the Sprain?
If you’ve sprained your ankle you will most likely experience pain, swelling and bruising. Ankle sprains can range from mild to severe. The degree of pain and swelling will correlate to the severity of the sprain. If you have sprained your ankle badly, you may not be able to bear weight or walk on it. Getting your ankle evaluated promptly and beginning rehabilitation as soon as possible is very important. Patients who delay treatment or just limp along at home until their ankle stops hurting are more likely to have repeated sprains and possibly long-term, chronic ankle pain and weakness.
Repairing the Damage
If you have swelling and bruising along with pain after twisting your ankle it should be evaluated by one of our board certified foot and ankle surgeons, Dr. Victoria Foley or Dr. Constance Omelas. After examining your ankle, the foot doctor will most likely want you to have a digital x-ray (which can be done conveniently right in our Long Beach office) to rule out a fracture, which can happen at the same time as a sprain. Once the podiatrist has assessed the degree of injury, an appropriate treatment plan can be developed.
The PRINCE Regimen
Until your appointment, you can care for your ankle using the PRINCE regimen:
Protection: Use a brace or other ankle support
Rest: Stay off your foot or avoid bearing weight by using crutches
Ice: Apply ice for 10-20 minutes every hour or two for the first 24 to 72 hours
Nonsteroidal anti-inflammatory medications: Ibuprofen or acetaminophen for pain relief
Compression: An ACE bandage or elastic compression wrap for the first 24-36 hours will help reduce swelling
Elevation: Keep your ankle above the level of your heart for 2-3 hours a day if possible
To get your ankle checked, contact us at: 562-420-9800 as soon as possible after the injury occurs.
Give Your Feet the Care They Deserve
According to the American Podiatric Medical Association, most Americans will have put 75,000 miles on their feet by the time they reach the age of 50! Although in some ways our lives have become more sedentary than in previous generations we now engage in much more rigorous fitness activities to compensate then in times past which can mean even greater wear and tear on feet and ankles. Take running, for example, which puts pressure on each foot equivalent to 3 to 4 times the weight of your body. Even walking for a person who weighs 150 pounds will exert an estimated 127,000 pounds of pressure per foot per mile. At Superior Foot & Ankle Care Center we want to share these figures to help you gain more respect for your feet and the importance of caring for them. Your feet are wonderfully made complex structures comprised of 26 bones, 33 joints and more than 100 muscles, tendons and ligaments. You can help keep your feet healthy and prevent many common problems by following a few footcare basics:
- Develop a regular care regimen. Wash feet daily and dry thoroughly (especially between the toes). Apply a rich moisturizer to keep skin supple and hydrated. If you tend to sweat excessively, use a talc or anti-fungal foot powder as well.
- Make good shoe choices. Poorly fitting shoes are one of the biggest causes of foot problems. Be sure that toes are not squeezed and that the shoes you wear provide good arch and ankle support. Avoid overly high heels and discard shoes when they are worn out.
- Exercise wisely. Being fit is important for your feet and the rest of your body too. Regular exercise is recommended but be sure to start gradually and work up to longer and more intense workouts in order to avoid injury.
- Inspect your feet periodically. Look for changes in size, shape, skin color or temperature as well as any lumps, bumps or unusual changes in your toes. Most foot problems are more successfully treated and with less invasive means if caught in the early stages. Report anything suspicious to your foot doctor.
- Don’t ignore pain in your feet—it’s never normal! Our board certified podiatrists, Dr. Victoria Foley and Dr. Constance Omelas will conduct a thorough examination of your feet and diagnose the source of your pain. A custom treatment plan will soon have you on track to getting back to the active lifestyle you normally enjoy. Contact our Long Beach office by calling: 562-420-9800 for an appointment.
Skin Cream and Your Feet
Do you ever have those mornings when you’re in a rush, so you don’t have all the time you need to properly perform your skin care regimen? On one of those mornings have you ever secretly used your hand or foot skin cream on your face?
You probably think “What’s the harm?” Here’s a look at why all skin creams aren’t the same and what you should be using to treat dry feet.
Skin Cream: Is Each One Equal When It Comes to Your Feet?
The simple answer is no, not all skin creams are created equal because each skin cream is designed to treat specific areas of the body. By their nature, the skin of your face and that of your hands or feet aren’t the same. The skin on your face is more delicate, while the skin on your hands and feet is thicker. Skin is actually different everywhere, which means different care and different formulas.
Hand and foot creams may have the same basis as face creams, and they have ingredients in common, but they have different concentrations of them, which is what makes all the difference.
Hand and foot creams need to work as barriers. For this, they need to have high concentrations of wax, greases, oils, and chemical exfoliating agents. If you use them on your face, you risk causing blocked pores and pimples. So, while you can use a face skin cream on your feet or your hands, you shouldn’t do it the other way around—even if you have a tiny dry patch. Foot and hand creams are just too rich, thick, and sticky to be applied to your facial skin.
Treating Dry, Cracked Feet at Home
With the cold weather just over the horizon, so too are dry feet. Here are some tips on how you can treat dry, cracked feet at home:
- Wash feet daily with warm, soapy water. Don’t use hot water because it dries out skin. Hot water is also harmful to diabetics and anyone else with impaired circulation to the feet.
- Exfoliate the feet, especially the heels, while washing. Use a warm cloth or pumice stone, and rub the skin gently to slough off dead skin.
- Dry feet thoroughly. Dry well between the toes since fungus and bacteria like to grow in warm, moist, dark places.
- Moisturize daily. Try using products containing urea, which is naturally present in skin cells. Using a product that has urea increases the skin’s ability to hold in moisture. Avoid moisturizer between the toes. Put on cotton socks after moisturizing.
- Soak your feet. Limit foot soaks to 10-15 minutes, three times a week. Soaking for long periods of time can dry out your feet. Use a solution of ¼ cup white vinegar and enough warm water to cover the feet up to the ankles. The mild acetic acid in vinegar softens skin.
Making Your Own Moisturizer
Here are some easy home-made moisturizers that can help heal dry, cracked feet.
Coconut Shea Butter—combine ¾ cup coconut oil with ½ cup shea butter in a sauce pan and place on low heat. Once they’ve melted, remove from the heat and stir in 15 drops of lavender essential oil. Store in a glass jar with a lid somewhere cool. Massage this foot moisturizer into feet, focusing on dry, cracked areas. Cover feet with cotton socks right away. Try this once in a while for some nice pampering or repeat on a regular basis to soften dry feet.
Honey Foot Cream—warm 1 cup of organic honey slightly to make it easier to spread. Stir in 2 tablespoons of warm milk and the juice of ½ an orange. Use a pumice stone or foot file to slough off some of the callused skin before spreading a layer of mixture evenly onto your heels, massaging as you go to help it sink in. Leave it on for 45 minutes and then rinse with warm water and dry thoroughly. Do this twice daily. If you prefer, you can apply this skin cream before bed and let it dry and then leave it on overnight.
Treating Dry Feet
If you are concerned about having dry feet or have any questions about what products are safe to use on your feet, then you should book an appointment with Dr. Vikki and Dr. Connie of the Superior Foot and Ankle Care Center. With years of collective experience in their field, they will be able to help you find the best products to use on your feet.
Hammertoes: Everything you Need to Know
If you’ve noticed that your toes have been looking a little strange to you lately, or that they have become unusually rigid and tight, you may have hammertoes. A hammertoe is as unpleasant as it sounds: as the namesake suggests, a hammertoe is a deformity which causes the toes to bend sharply downwards rather than straightforward, resembling the silhouette of a hammer.
It is a common but painful condition affecting over 200,000 Americans per year, typically resulting from years of wearing ill-fitting shoes with narrow toe boxes, such as fashionable heels. Fortunately, hammertoe is easily diagnosed and treated, if you know what to look out for. Here is a look at hammertoe causes, symptoms, and treatment:
What Is Hammertoe?
While hammertoe can affect any of the toes, it is most commonly seen afflicting the second, third, or fourth toe. This deformity results when the middle joint of the toe becomes dislocated, forcing the toe to bend sharply downward and buckle in this position. The underlying cause is a muscle and ligament imbalance surrounding the toe joint, where the muscles have tightened from being forced into a flexed position – such as when wearing cramped shoes – to the point where they can no longer straighten out. Pain can result from excessive friction and rubbing against the top of the deformed toe, and corns and calluses may form to further exacerbate the condition.
A number of factors can contribute to the development of hammertoe:
- An uncommonly high foot arch
- Flat feet
- Cramped or ill-fitting shoes
- Pressure from a bunion
- Toe injury
- Arthritis
- Tight tendons or ligaments in the feet
Symptoms & Diagnosis of Hammertoes
Hammertoe is easily recognizable, but you’ll want to confirm with a podiatrist for an official diagnosis. Common symptoms which indicate hammertoe include:
- Pain when walking
- Pain when stretching the affected toe
- A toe which bends downwards and is difficult to move
- Difficulty wiggling the toes or flexing the foot
- Calluses or corns
- Toes taking on a claw-like appearance
There are two types, or stages, of hammertoes: flexible and rigid. A flexible hammertoe means that the condition was caught within its early stages, where the toe is still able to move at the middle joint. This form of hammertoe is still mild, and has a number of various treatment options available. When the condition progresses to the point where the tendons become rigid enough to push the joints out of alignment, the toe will become immovable. At this stage, surgery is usually required.
Your podiatrist can often visually diagnose hammertoe with a physical exam. However, if you’ve had a toe injury, imaging tests may also be required.
Hammertoe Treatment & Prevention
The course of treatment depends upon how far your hammertoe has progressed.
Mild hammertoe that has been caught in its early stages and still remains flexible has a much greater variety of treatment options available. The first step is identifying the cause responsible for the hammertoe. If cramped footwear is the issue, simply switching to better shoes can remedy the condition. If flat feet or high arches are to blame, custom insoles or toe pads can offset the damage. For corns, over-the-counter medications or pads may suffice. Again, consult a podiatrist to determine the source of your hammertoe, to properly advise you on the appropriate treatment option.
Severe hammertoe that has become rigid and inflexible will require surgical intervention to restore motion to the toe. Hammertoe surgery may involve repositioning of the toe, removal of damaged bone, and realignment of the tendons.
The best prevention tip for hammertoes is to make sure that your shoes are fitting properly, and that your feet’s special needs are met. This means getting insoles or orthotics if you require them, and ensuring that your shoes are not too snug nor the heels too high. In general, it is recommended to avoid any heel over 2 inches in height. If you notice any pain, discomfort, or deformity, consult a podiatrist at your earliest convenience to avoid further complications.
Schedule a Consultation with Dr. Vikki and Dr. Connie
If walking has become painful and you suspect that hammertoes are to blame, schedule a consultation with trusted podiatrists Dr. Vikki and Dr. Connie at the Superior Foot & Ankle Care Center today.
Feet Facts You May Not Have Known About
A trivia question: What is the best exercise for your feet? (The answer can be found at the end of this article.)
The likes of Stephen Hawking, Theodore Roosevelt, and Abraham Lincoln have all employed the feet metaphor in some of their most inspiring quotes, underscoring the literal and figurative significance of paying attention to our feet. And yet, so many of forget to do so. This is a shame, as our feet are more fascinating than most of us realize.
Fun Feet Facts
The University of California, Berkeley, has a list of facts about our feet that are worth our time knowing about – not just for the sake of curiosity, but even to better inform how we look after our feet:
- Each foot contains 26 bones (with both feet together having more than one quarter of the body’s total bones); 33 joints; and more than 100 tendons, ligaments, and muscles.
- There are more than 100,000 nerve endings in each foot, which provide sensory feedback to your brain, enabling you to automatically adjust your gait according to your environment to reduce impact forces on your body. Wearing shoes alters this feedback mechanism.
- Each foot has about 125,000 sweat glands, which combined excrete more than a cup of perspiration a day (no wonder feet sometimes don’t smell so good).
- A person who averages 8,000 to 10,000 steps a day (the minimum recommendation for overall good health) will, over a 75-year lifetime, walk the equivalent of circling the world three times.
- During high-impact activity, the forces on your feet can be equal to twice your body weight—or even more.
Additional Bonus Facts
- Toenails take longer to grow than fingernails do. It takes approximately a year and a half to grow an entire toenail. In addition, research shows that being younger, male, and/or a nail biter could all be driving factors in having a faster nail growth rate.
- Osteoarthritis is the most common type of arthritis, affecting an estimated 20.7 million adults in the United States.
- The average American walks 5,900 steps a day. The recommended daily number of steps is 10,000, which is approximately five miles.
- Cigarette smoking increases the risk of peripheral arterial disease (PAD) by several folds and is one of the most prominent risk factors. PAD is a disease in which plaque builds up in the arteries that carry blood to your head, organs, and limbs and usually affects the arteries in the legs, leading to pain and numbness in the lower extremities. In severe cases, PAD may cause infection, gangrene, and lead to leg amputation.
- When our feet are misaligned, the effects can be felt in the muscles in the rest of the body, potentially causing joint pain or even serious injuries. There are two types of foot misalignment: overpronation and excessive supination. Over 75% of the population suffers from foot misalignment.
- Ankle sprains are one of the most common injuries in sports. Because the inner ankle is more stable than the outer ankle, the foot is likely to turn inward from a fall (ankle inversion) which results in an ankle sprain.
- More than one-third of women in America have bunions, a common foot deformity in which the joint that connects the big toe to the foot gets larger and juts out.
- Both Michelangelo’s David and the Statue of Liberty have Morton’s toes. It’s is a foot condition in which the second toe is longer than the big toe. It is also called Greek foot because the ancient Greeks found it aesthetically appealing and incorporated it into paintings and sculptures.
- The feet can contract an array of nasty diseases from communal showers: Plantar warts, athlete’s foot, and ring worm are just some!
And the answer to the trivia question is walking. Walking contributes to your general well-being and improves circulation and weight control.
Remember to look after you feet. If you’re worried you may have foot health issues, get in contact with Dr. Vikki and Dr. Connie today.
Modern Marvel of Prosthetic Feet
If you’re fortunate enough to have all of your limbs, then chances are you take them for granted. Prosthetic limbs, such as feet, are incredibly valuable to amputees because a prosthetic can help restore some of the capabilities lost with an amputated limb. Although prosthetic limbs have still not advanced to the point where they can rival the functionality provided by biological limbs, the capabilities they do provide can be significant.
Here’s a quick look at how prosthetics work to make life easier for amputees.
How Prosthetics Work
While new materials and technologies have modernized prosthetics over the past century, the basic components of prosthetic limbs remain the same. The basic components include:
- The pylon—the internal frame of skeleton of the prosthetic. The pylon provides structural support and has traditionally been formed of metal rods. However, modern technology has allowed for lighter carbon-fiber composites to be used in place of the metal rods. The pylons are sometimes enclosed by a cover (usually made from a foam-like material). The cover can be shaped and colored to match your skin tone in order to give the prosthetic a more lifelike appearance.
- The socket—the portion of the prosthetic device that interfaces with the patient’s limb, stump, or residual limb. Since the socket transmits force from the prosthetic to the body, it must be meticulously fitted to the residual limb to ensure that it doesn’t cause irritation or damage to the skin or underlying tissues. A soft liner tends to be used in the interior of the socket, and a patient may also wear one or more prosthetic socks to achieve a snugger fit.
- The suspension system—this is what keeps the prosthetic attached to the body. The suspension mechanism can come in several forms (straps, belts, or sleeves), although the most common type of suspension mechanism relies on suction.
Even though most prosthetic limbs have these basic components in some form or another, each device is unique and designed for a specific type and level of amputation.
Choosing the Right Prosthetic Foot
Today, amputees have a wide variety of prosthetic feet to choose from, designed for walking, cycling, golfing, swimming, snow skiing, and running. Heavier wood and steel materials have been replaced by lightweight plastics, aerospace alloys, and carbon-fiber composites. But how do you choose the right one for your lifestyle?
There are a number of key factors that you should consider, including materials, comfort, function, energy storage, and multi-axial motion.
- Materials—the materials in a prosthetic foot differ by activity level. Wood, plastic, and foam are usually found in feet designed for people with low activity levels and for those who require stability. Carbon feet meet the functional needs for shock absorption and energy efficiency, and are also lightweight.
- Comfort—a prosthetic foot has to feel good for you to meet your activity goals. Comfort allows you to be more active, and the function of your prosthetic foot directly affects comfort.
- Function—prosthetic feet are designed to mimic the human foot at a specific activity level. For people who can’t walk, the function is largely cosmetic. For those who are most active, a prosthetic foot must mimic a normal foot during the act of walking. It must act as a shock absorber when your heel hits the ground, adapt to uneven terrain, provide a smooth rollover from heel to toe, and provide a rigid lever for propelling forward when you finish your step.
- Energy storage—a foot made with carbon fiber for energy storage gives you a spring in your step as the carbon fiber acts as a spring, compressing as you apply weight and propelling you forward as your foot rolls, returning energy to your step as the spring releases. Some prosthetics have one spring in the heel and a second spring in the forefoot (just what you need for walking in various speeds, running, climbing hills, or descending stairs with a secure, confident stride). With carbon fiber, the longer the spring, the more energy it can store and the more responsive the foot will be.
- Multi-axial motion—some prosthetic feet are designed to mimic the ankle, which allows the foot to move in multiple planes. Multi-axial capability in a foot allows you to raise and lower the forefoot, move the forefoot to the left and right, and roll the foot slightly to the inside or to the outside. Multi-axial motion is needed to walk comfortably and confidently on uneven ground, when your foot must adapt to whatever it encounters.
The Bionic Foot
While prosthetics are the norm for amputees at the moment, the future seems to be leading us in the direction of bionic feet. Bionic feet that can be controlled by the patient’s mind, using sensors implanted inside the muscle tissue, have been proven to work in human-testing trials.
The tiny implanted myoelectric sensors (IMES), which are surgically implanted in the residual muscle tissue about the leg, wirelessly transmit a signal to the foot, telling it to perform a specific action. While this is a breakthrough in prosthetic technology, there are still a few bugs to work out before this becomes a more mainstream option for amputees.
Schedule an Appointment
If you have any questions or concerns about foot health or need guidance in the event you’re in need of a prosthetic foot, do not hesitate to contact the caring and professional team at the Superior Foot and Ankle Care Center.
The Top Health Benefits of a Regular Foot Massage
Massage therapy has long been lauded as an effective treatment for relieving muscle tension, pain, and stress, but research suggests that the scope of its health benefits go much further. While there are different schools of massage therapy, from Swedish massage to shiatsu, all schools involve applying various levels and techniques of pressure to the muscles in order to promote relaxation. When performed by a trained professional, massage therapy can help resolve muscle damage and even prevent injury.
Foot massage is especially important, as the feet are among the most overused and under-cared for parts of the body. Foot massage techniques are deeply rooted in the study and traditions of reflexology, an alternative medicine discipline that focuses on stimulating pressure points in the feet which correspond to specific systems in the body.
The proven stress reduction stemming from reflexology techniques is then extended to alleviating the symptoms of various ailments and conditions. While a foot massage in itself may not be a cure-all, its stress-relieving and muscle-soothing benefits have far-reaching positive effects on your health, from improved circulation to better sleep.
Here is a look at a few reasons why you should schedule a foot massage regimen:
Stress Relief
The strength of massage therapy as a treatment lies in the healing power of the human touch.Massage reduces the levels of cortisol in the body, the hormone responsible for the negative impact of stress. Moreover, massage has also been shown to improve the levels of serotonin and dopamine which are central to depression. Studies have also found massage to be correlated with increased levels of oxytocin, the hormone intrinsic to emotional bonding.
Thus massage not only relieves the physical tension associated with stress, but the sensation of repeated human touch given in a safe environment produces positive emotions proven to improve symptoms of depression and anxiety. But don’t feel restricted to a professional massage therapist: the emotional benefits associated with massage are just as – if not more – accessible when performed by a loved one.
The benefits of this stress release are expansive: massage can be used as an effective treatment for conditions in which depression and anxiety are the primary symptoms, for example the hormonal changes experienced during PMS and menopause. For this reason, massage has also proven useful in treating migraines and headaches caused by chronic stress. While massage isn’t intended to replace medication for a condition in which depression is a symptom, it is an extremely effective therapy to supplement medical treatment.
Improved Circulation
A 10-20 minute foot massage before bed can work wonders in improving your blood circulation. The kneading pressure applied during a massage helps to improve blood flow through congested areas, allowing fresh blood to flow in. The motions of squeezing and pulling work to clear the muscles of lactic acid, while improving lymph circulation to clear your system of metabolic waste. Better circulation improves blood flow, lowers blood pressure, and enhances overall body function. This is especially helpful for diabetic patients, who struggle with poor circulation in their lower extremities.
Relieves Pain While Reducing Injury
Just 10 minutes of massage following a workout can help reduce inflammation, allowing your body to recover more effectively. Combining strengthening exercises, stretching, and regular foot massages not only facilitates the recovery of existing foot injuries, but helps prevent new injuries from occurring.
Moreover, regular foot massage with deep pressure applied to the arch can alleviate the pain associated with any deformity or weaknesses in the foot, such as with flat feet and plantar fasciitis.
Better Sleep
Due to its expansive stress relieving benefits, foot massage has also been shown to enable relaxation and improve sleep in patients who find it difficult to rest otherwise. This includes individuals who are under chronic stress or struggle with insomnia. Massage therapy has even been shown to improve the rest of patients undergoing chemotherapy. New parents will also be pleased to find that basic massage techniques can even work on newborns, coaxing finicky infants to sleep.
Schedule a Consultation with Dr. Vikki and Dr. Connie
Don’t wait until your foot health is compromised to take advantage of the benefits foot massage has to offer. Schedule a consultation with trusted podiatrists Dr. Vikki and Dr. Connie at the Superior Foot & Ankle Care Center to learn more today.
Prehensile Feet: People With Feet Similar to Monkeys
Despite the way our species evolved away from climbing trees to walking on flat ground, some people are still walking around with monkey-like feet. In fact, you may be surprised to learn that about eight percent of the population, or 1 in 13 humans, may have a midtarsal break in their foot characteristic of non-human primates. These are also referred to as prehensile feet.
What is a Midtarsal Break?
The midtarsal break is a medial shift in the center of the pressure trajectory with dorsiflexion of the midtarsal joint (the joint between the talus and the navicular bone as well as the joint between the calcaneus and the cuboid bone), occurring during the gait of an unstable foot, when the body transfers weight from rearfoot to forefoot.
A midtarsal break, also known as floppy feet, tend to occur in people with flatter feet and higher body mass indexes than people with stiffer feet. They also tend to roll their feet more, causing a motion called hyperpronation (they land on the outside of their feet and roll dramatically inward). This allows for the foot to relax its joints and ligaments, creating a midtarsal break.
What are Prehensile Feet?
Prehensile feet are lower limbs that possess prehensility (the ability to grasp like a hand). They are most commonly observed in monkeys. Due to the development of bipedalism in humans, the hands became the focus of prehensility and the feet adjusted to more of a stabilizing role. It may be possible, however, that the foot does not reach its limits of dexterity due to the constant muscle tension needed in stabilizing and balancing the foot to hold up the legs and the rest of the frame.
People with prehensile feet can grasp small objects between their toes, manipulating them as with a hand with the ankle functioning like the wrist. As toes are much shorter than fingers, and since the ball of the foot is so large and obtrusive, grasping does not function as in a normal hand and the foot is not able to hold very large or heavy objects.
Chimpanzee Feet vs. Human Feet
Conventional wisdom has always claimed that the human mid-foot is rigid, which allows for more efficient walking while chimpanzees and other apes have flexible feet better suited to grasping branches as they move through the trees.
Human feet are both rigid and pliable depending on the need. The human foot is a spring arch that should be able to drop and lift with every step. Human legs angle in from the hip to the knee, allowing our feet to fall directly under the pelvis and our pelvic muscles are much stronger, as well, allowing for a stable upright environment.
Chimpanzees are often referred to as knuckle-walkers because they only walk on two legs for short distances due to the differences of our legs and spine. Chimpanzees can’t straighten their legs like humans and they don’t have a lumbar curve, which makes weight bearing and walking more difficult. Chimpanzee legs are also set wide apart and weak pelvic muscles force their whole body to transfer weight from side to side during each step.
Yet, while chimp feet and bodies can’t do what humans can, it doesn’t appear to be a problem if our feet work like chimpanzee feet. In fact, two studies (one from Boston University and the other from Dartmouth) have proven that about eight percent of the population have the mobility of chimpanzee feet, which allows some societies to functionally adapt their feet and calf muscles to allow them to climb trees like chimps do.
While eight percent of the population exhibits a flexible midtarsal break in their feet, people with midtarsal break rarely realize that they have one, as it doesn’t affect their gait.
The Walking Test
So how do you know if your feet might have a midtarsal break? Take a stroll on sand. Here are a couple of tips:
- If you have high arches, you probably have stiff muscles and ligaments, which means that you don’t have a midtarsal break.
- If you have a midtarsal break, the fold in your foot will pinch the sand upward. Look for a small ridge in the upper-mid portion of your footprint.
Talk to Dr. Vikki and Dr. Connie
If you have any questions or concerns about whether or not you have prehensile feet with a midtarsal break, and if there are any unique factors you have to account for regarding your foot health, feel free to book an appointment with Dr. Vikki and Dr. Connie today.