Connect With Us
Blogs

Diabetes (10)
November is American Diabetes Month and at Superior Foot & Ankle Care Center this is a topic of high importance. Diabetes has the potential to seriously impact the health of your feet. When blood sugar levels are high, your immune system can be compromised, and your body may have difficulty fighting infections. Two other conditions associated with diabetes—poor circulation and peripheral neuropathy (loss of feeling) — can conspire to put your feet at risk for dangerous wounds and infections. Diabetes can also affect your bones, joints, and skin. This year’s message from the American Diabetes Association, however, is one of hope: “We Stand Greater Than Diabetes.” The good news is that there are many ways to prevent podiatric problems if you have diabetes. Below are eight to consider:
- Schedule regular podiatric exams. Our podiatrists, Victoria M. Foley and Dr. Constance Ornelas, are an important part of your health care team if you have diabetes. Seeking care regularly will help the foot doctor spot problems before they get out of control and help you be proactive in protecting your feet.
- Check your feet daily. Getting in the habit of examining your feet—top, bottom, between the toes and toenails—will enable you to spot any changes promptly. Cuts that aren’t healing, redness, swelling, bruising, growths, or changes in skin color or nails may all be signs that something potentially harmful is developing. Any changes should be reported promptly to our Long Beach office by calling: (562) 420-9800.
- Choose your shoes carefully. Avoid stiff shoes and look for styles that have roomy toe boxes. Get your feet measured and fitted professionally and periodically run your hand around the inside of the shoes to make sure there are no rough seams or material that could cause friction and blisters.
- Don’t smoke. It impedes circulation.
- Keep feet dry. Sitting in damp footwear can increase your risk of athlete’s foot and fungal toenails.
- Don’t go barefoot. Even at home, wear slippers or shoes to prevent cuts and puncture wounds.
- Do not use medicated pads, acid solutions, or sticky pads. For warts, corns, and calluses consult your podiatrist for treatment and don’t attempt any “bathroom surgeries.”
- Follow your doctor’s instructions for managing your diabetes. Take your medications as directed, eat a nutritious diet, maintain a healthy weight, and exercise regularly.
During the month of August, we at Superior Foot & Ankle Care Center recognize Psoriasis Action Month. Psoriasis can appear on your legs and feet as well as on other parts of your body. Below are some facts about this condition and what can be done about it.
FACT: Psoriasis is a chronic disease of the immune system. It manifests most often as a skin condition. In people with psoriasis, new skin cells come to the surface too rapidly. This results in an inflammation of the skin.
FACT: It’s estimated that 8-12 million Americans currently suffer from psoriasis.
FACT: Psoriasis often first develops in patients between the ages of 15 and 25, but can strike at any age.
FACT: Researchers believe that the cause of psoriasis is a combination of an inherited genetic tendency for the disease combined with exposure to certain external triggers. Several possible triggers have been identified, including stress, certain medications, an injury or infection. Triggers are not the same for each person.
FACT: There are multiple types of psoriasis and they can appear differently on the skin. Thick patches of skin, redness, blisters, and lesions are some of the possible symptoms. Psoriasis may cause itching and pain.
FACT: Psoriasis can also cause inflammation and pain in your joints, tendons, and ligaments. About one in three patients with psoriasis develop psoriatic arthritis.
FACT: Patients with psoriasis are at an elevated risk for contracting other conditions like cancer, cardiovascular disease, depression, osteoporosis, liver disease, diabetes, and more.
FACT: On your feet and toenails, psoriasis may look like athlete’s foot or fungal toenail infection. For this reason, if you notice any unusual changes in your skin or toenails or you are experiencing unexplained joint pain, contact our Long Beach office by calling: (562) 420-9800 for an appointment. Our podiatrists, Dr. Victoria M. Foley or Dr. Constance Ornelas will examine your feet and determine whether an infection, psoriasis or some other disorder is the source of your discomfort.
At Superior Foot & Ankle Care Center, we know that diabetes can affect your skin, joints, and bones in a number of ways. Two conditions associated with the disease—peripheral arterial disease (PAD) and neuropathy—are of particular concern when it comes to your lower extremities. PAD is a narrowing or blocking of the arteries to your legs, which can lead to poor circulation. This means that nutrient and oxygen-rich blood necessary for healing cannot reach your legs, feet, and toes as quickly as needed. Neuropathy is nerve damage that can result in loss of feeling in your feet, which makes it difficult to perceive pain and injury. This double whammy means that patients with diabetes are at a higher risk for a host of podiatric problems, including:
- Ulcers and wounds that do not heal properly
- Fungal infections
- Hammertoes
- Ingrown toenails
- Corns and calluses
Difficulty healing can cause even minor foot and toe problems to become major threats with the potential for infection and even amputation. Below are some ways you can be proactive in preventing foot problems if you have diabetes:
- Control your blood sugar. Follow all your doctor’s instructions for managing your diabetes. Watch your diet, take your medications as directed and regularly test to make sure you are on track.
- Schedule regular podiatric checkups. Our podiatrists, Victoria M. Foley or Dr. Constance Ornelas, will work with you to prevent potentially dangerous foot issues. Seeing the foot doctor regularly will increase the chances of catching injuries and infections in their very early and most treatable stages. The podiatrist can also help with nail care, wound debridement and diabetic footwear and orthotics.
- Keep feet clean, warm, and dry. Wash daily and dry thoroughly—especially between your toes. Use a foot powder before putting on socks.
- Make sure shoes fit correctly. Avoid styles that have narrow toe boxes are that are made of very stiff materials. Keep the heel height to 2 inches or less.
- Don’t walk barefoot. This dramatically increases your chances of getting athlete’s foot or a fungal toenail infection, which are contracted by direct contact. You are also more likely to step on a sharp object and injure your foot without shoes.
- Conduct regular self-exams—it’s important that between appointments you are checking your feet and toes daily for any signs of rashes, cuts, blisters, bruises, growths or other indicators that a foot problem is developing. If you can’t see your whole foot as a family member or caregiver to assist you. Contact our Long Beach office immediately by calling (562) 420-9800 if you find anything concerning.
Did you know that the leading cause of lower extremity amputations not caused by trauma is diabetes? And, foot ulcers precede 85 percent of these amputations. At Superior Foot & Ankle Care Center we want patients to know that diabetic foot ulcers can be prevented and our podiatrists, Dr. Victoria Foley and Dr. Constance Omelas will work with you to develop a care regimen and monitor your feet as a diabetic patient. Adhering to a schedule of regular podiatric checkups is an important step in protecting your feet if you have diabetes. Below are other areas where you can be proactive in preventing ulcers:
Healthy Foot Habits—in addition to regular podiatric exams, doing your own self-exams at home is also very important. Foot ulcers commonly form on the soles of the feet so be sure you check the bottom of your feet carefully (or have someone do it for you) and the rest of your feet as well on a daily basis. Report any redness, sores, blisters, rashes or cuts to the foot doctor asap. You should also wash your feet daily and dry completely. Use foot powder and change your socks whenever you notice that your feet feel damp. This will reduce the risk of bacterial and fungal conditions which can lead to infections and wounds.
Footwear—the shoes you wear can play a big part in preventing conditions that can lead to wounds. Choose styles that are made of soft, flexible material and have wide, roomy toe boxes. Shoes that squeeze toes together can increase the risk of ingrown toenails and blisters and hasten the progression of toe problems like hammertoes and bunions. Periodically run your hand around the inside of your shoes to make sure there are no small pebbles stuck inside or loose stitching that can rub against the skin and cause an irritation.
Lifestyle Choices—one of the most important steps you can take for preventing ulcers is keeping your blood sugar levels where they should be. Follow the dietary plan your doctor has given you and fill your menus with nutrient-rich foods that are low in sugar. Don’t smoke because it impedes circulation. Limit alcohol use as this has been linked with an increased risk of foot ulcers.
If you have diabetes and have additional questions about how to best care for your feet and prevent diabetic complications, contact our Long Beach office by calling: (562) 420-9800.
Before we say goodbye to the month of June, there’s one more health observance that we at Superior Foot & Ankle Care Center want to acknowledge: Men’s Health Month. A significant amount of research has been done about men and one disease that is of particular interest to us as foot health care providers, and that is diabetes. Although men and women may have similar symptoms and treatment, studies have shown that overall how men respond to diagnosis and care of the disease is very different and not in a good way.
The First Step: Admitting There’s a Problem
For many men, even after they realize that something is not right with their feet they put off making an appointment to have their symptoms evaluated. The reason for this is that they are afraid of getting bad news. If you are a man (or someone who loves one) and have noticed any of the following symptoms in the feet: cuts that are slow to heal, loss of sensation in one or more parts of the feet or a burning, tingling feeling, swelling or anything else out of the ordinary, it’s important that you make an appointment at our Long Beach office and allow one of our podiatrists, Dr. Victoria Foley or Dr. Constance Omelas to examine your feet. Delaying seeking treatment will not make the symptoms go away and prompt treatment can greatly improve the outcome.
Get the Care You Need
Another significant research finding showed that in cases where men and women had equal access to health care for their diabetes, men were more likely to miss appointments and not get the treatment they needed. The good news about diabetes is that is highly controllable today. Many patients with diabetes continue to live full and active lives—if they keep their diabetes under control. The best ways to do this are:
- Schedule (and keep!) regular appointments with the podiatrist and other physicians managing your diabetic care.
- Follow dietary recommendations and medical treatments.
- Check your feet daily for changes that may indicate a problem.
- Wear shoes that fit properly and allow plenty of room in the toe box.
- Keep feet dry and avoid putting them in front of direct heat.
At Superior Foot & Ankle Care Center we can take the fear and mystery out of diabetes if you let us. If you have concerns about your feet (or you believe a man in your life does) contact us by calling: (562) 420-9800.
Here at Superior Foot & Ankle Care Center we believe in the importance of good foot care for all or our patients. For those with diabetes, however, extra precautions are necessary. Diabetes has several conditions associated with it that can result in major medical complications being caused by what other patients may deem minor foot issues. A compromised immune system, reduced circulation and neuropathy (or lack of sensation) all require additional measures to keep feet safe and healthy. Below are 6 podiatric tips for patients with diabetes:
- Choose footwear carefully. Shoes should have roomy toe boxes that don’t cramp or squeeze toes together. This will reduce the risk of ingrown toenails. Shoes should be made of natural, breathable materials. Inspect shoes periodically to make sure there are no rough spots, loose stitching or other elements that could rub on the skin and cause a blister or ulcer.
- Watch the heat. Don’t expose feet to high temperatures from fire places or electric blankets. Carefully monitor water temperature in baths and showers. A loss of sensation can result in burns due to the fact that the patient does not perceive pain from heat or burning.
- Stay dry. Fungi love moist, dark places to grow, such as the inside of sweaty socks. Change socks as soon as you notice they are damp to help avoid fungal infections.
- Keep the blood flowing. You can help improve circulation by exercising regularly and not sitting or standing in one position for long periods of time. Don’t cross your legs or wear socks that are tight or have elastic in the top to hold them up.
- Inspect feet daily. Wash your feet in warm soapy water every day and while you do so, check for cuts, blisters, bumps, bruising, swelling, growths or anything unusual or different on your feet. Report any changes to the foot doctor promptly.
- Make your podiatrist a care partner. Regular podiatric checkups with our podiatrists, Victoria M. Foley and Dr. Constance Ornelas can go a long way toward prevent footing health problems. If seen regularly, the foot doctor can detect changes and potential issues in your feet in the very earliest stages and stop problems before they start.
If you are a patient with diabetes and you have questions about the health of your feet, contact our Long Beach office by calling: 562-420-9800.
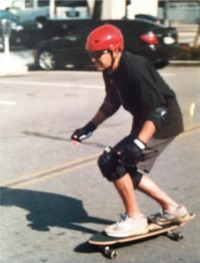
Meet Joe Plank: He’s 81 years old and loves to skateboard! A Long Beach resident, Joe works as a grief counselor at the VA, helps autistic children in the county of Orange and enjoys lots of activities with his daughter and her family. Joe also has diabetes. As a patient of Superior Foot & Ankle Care Center, we see Joe as living proof that diabetes doesn’t have to stop you from living a full and (very!) active life.
One of the best ways to help control your blood sugar is through exercise. In addition, many diabetic patients suffer from neuropathy and circulation issues. Exercise is an excellent way to keep the blood flowing. Before skateboarding, Joe was an enthusiastic surfer for more than 6 decades. Although the activities that you choose may change over time, it’s important to make exercise and fitness a lifelong habit. Our board certified foot and ankle surgeons, Dr. Victoria Foley and Dr. Constance Omelas can make recommendations of activities and footwear that would best suit your feet and ankles. Your podiatrist can also tell you other ways to help take care of your feet if have diabetes. A few items that should be on your daily foot care regimen checklist include:
- Wash feet with a mild soap and warm (not hot) water. Dry completely, especially between the toes (to help prevent athlete’s foot).
- Inspect your feet, toes and ankles for changes. Look for swelling, cuts, bruising, changes in color, shape or size, bumps, rashes or blisters. Report anything unusual to the foot doctor immediately.
- Apply a rich moisturizer to keep feet supple and prevent skin and heel cracks.
- Keep toenails cut straight across and not too short to prevent ingrown nails from developing.
If you want to learn more about diabetic care and how to maintain an active lifestyle with this disease, contact our Long Beach office. And, be sure to wave to Joe if you see him skate boarding at Huntington Beach Pier. Remember, as Joe says, “Being a geezer is a conscious choice.”
Did you know that more than 60% of all non-traumatic lower limb amputations are the result of complications from diabetes? The good news, however, is that you can reduce your risk of amputation by up to 85% and of other diabetes related foot problems as well by partnering with you podiatrist. November is National Diabetes Month and we at Superior Foot & Ankle Care Center want to help you prevent foot health issues commonly associated with diabetes.
Detecting Trouble Early
Neuropathy or nerve damage frequently affects patients with diabetes. Lack of feeling in your feet make it difficult to perceive pain, temperature changes and other signs that typically let your body know there’s a problem. As a result, sores and ulcers, calluses, infections and skin problems can all develop to a fairly serious level before being detected by the patient. One of the best steps you can take to prevent diabetic foot issues is to check your feet daily (or have someone do for you) for injuries or changes. Here’s what to look for:
- Changes in skin color
- Temperature changes
- Swelling of your ankle or foot
- Bruises, sores, cuts or red spots
- Dry skin, cracks in the heel or skin
- Corns, calluses and blisters
- Toenail changes—including discoloration, thickening, becoming ingrown
Avoiding Foot Issues
There are a number of ways to prevent diabetic foot problems from developing:
Visit Your Podiatrist–Diabetic patients should have two regularly scheduled exams annually with one of our board certified foot and ankle surgeons, Dr. Victoria Foley and Dr. Constance Omelas to check the health of your feet. In addition, if you notice any of the changes listed above, you should make an appointment immediately.
Wear Properly Fitted Shoes–It’s essential that shoes have a roomy toe box and enough room to prevent cramping and also so that no rubbing or friction against the skin occurs.
Don’t go Barefoot–Even at home, the risk of cuts, injuries and infections are too great.
Exercise–A moderate exercise program (approved by your physician) will help improve blood flow to the feet as well as control blood sugar and weight—all key for managing diabetes.
If you have more questions on diabetic foot care, don’t hesitate to contact our Long Beach office at: 562-420-9800.
Get the Facts on Foot Ulcers
Foot ulcers can develop into serious wounds and can even lead to the loss of a limb. This is why it is important to adequately treat every cut, callus and blister you sustain because they have the potential to develop into these serious foot ulcers. Here is some information about identifying, preventing and treating foot ulcers.
Who’s at Risk?
People who suffer from chronic illnesses such as sickle cell anemia, nerve damage from alcoholism, atherosclerosis (hardening of the arteries), and those with vascular issues can all be at risk of developing foot ulcers. However, the group that is most at risk are those with diabetes. This is because diabetics often suffer from peripheral neuropathy, which is nerve damage that numbs the extremities to cold, heat and pain.
Because of peripheral neuropathy, diabetics may sustain foot wounds that they are unable to feel and therefore do not treat. Walking around on untreated wounds will often cause them to become foot ulcers. Peripheral neuropathy can also cause the feet to become deformed. Putting deformed feet in normal shoes can cause blisters and calluses that may also develop into ulcers. In addition, diabetics often have poor blood circulation to their legs and feet and, without proper nourishment, the feet are unable to heal themselves of infections.
Identifying foot Ulcers
Foot ulcers are red sores found commonly on the balls of the feet or underneath the big toe. If they are infected, they will also produce pus and omit a bad odor. If left untreated, these sores can develop gangrene and your foot will eventually need amputation. For this reason, it is imperative to see a podiatrist if you suspect that you have a foot ulcer so you can be properly diagnosed and treated.
Preventing Foot Ulcers
- Inspect your feet regularly for cuts, blisters and calluses that can turn into ulcers.
- Keep your feet clean and well-hydrated.
- Exercise regularly, this improves your circulation.
- Keep your toenails trimmed properly.
- Don’t go barefoot because it leaves your feet vulnerable to harm.
- Don’t smoke because it weakens your immune system.
Treating Foot Ulcers
Cleansing and Debridement
Your doctor will cleanse the ulcer and remove any dead or dying tissue from the wound. An ointment that promotes healing may be added to the wound before your doctor bandages it.
Stay off Your Feet
Your foot may be put in a cast or protective boot. It is best to stay off your feet as much as possible while you are healing.
Assisted Wound Care
A foot care professional will have to inspect your ulcer once a week until it is fully healed. In addition, a visiting nurse will help dress your wound.
It is critical for diabetics to develop a good relationship with their podiatrists. Most diabetics will require regular care to assure that small problems will not develop into major issues.
Now that you know some facts about foot ulcers, be sure to reach out to a foot care professional if you suspect you have one. If you have any further questions about identifying, preventing or treating foot ulcers or want to book an appointment at the Superior Foot & Ankle Care Center, feel free to reach out to us.
You might be surprised to learn that many diseases have foot pain as one of their symptoms. Problems with the thyroid can cause nerve sensations in the feet; or degeneration in the lower back might irritate the nerves of the spine, impeding sensation in the feet. Learning what signs to look for could improve your life or even save it.
Peripheral Arterial Disease (PAD)
PAD occurs when plaque – a fatty substance which builds up in the arteries in the legs – reduces blood flow to the lower legs and feet. Symptoms include cramping in the calves, or other parts of the leg while it is in motion. It may even cause foot pain, or prevent wounds in the foot from healing properly.
While the most obvious symptoms of PAD involve the legs, it is associated with hidden damage to the heart and brain. This means that PAD sufferers are at a higher risk of heart attack and stroke. Smoking, diabetes, high cholesterol, and high blood pressure will also increase the risk of PAD. Medications may be prescribed, but diet and lifestyle changes are also necessary.
Rheumatoid Arthritis (RA) and Gout
The Arthritis Foundation revealed that 46 million Americans have arthritis or other chronic joint problems. Of the 1.3 million Americans who suffer from rheumatoid arthritis, 90 percent of them will experience symptoms in their foot and ankle.
RA develops when the body’s immune system mistakenly attacks the joints, causing pain and swelling. If RA reaches the feet, pain will begin in the toes, and then spread to the feet and ankles later on. The joint damage caused by RA can even change the shape of the toes and feet, given enough time. RA treatment involves medication, exercise, and sometimes surgery.
Gout is another type of arthritis caused by the accumulation of uric acid in the body. The acid collects in the joints, especially the big toes, and will cause intense, episodic pain. The acid may even cause kidney stones if it builds up there.
Gout treatment involves exercise, lots of water, avoidance of certain medications, and staying at a healthy weight. Doctors may prescribe gout patients with nonsteroidal anti-inflammatory drugs (NSAIDs), steroids, or other medications.
Diabetes
Approximately 24 million Americans have diabetes, but 6 million don’t even know it. Diabetes is a condition in which glucose, or blood sugar, builds up in the blood. While glucose is necessary to fuel the body, an excess amount will damage nerves and blood vessels in the feet, causing decreased sensation and reduced blood flow.
Other symptoms of diabetes include numbness and tingling in the feet, and severe foot infections. While many people experience foot discomfort after a long day of standing, severe foot pain out of proportion with your activity level is a problem that should be reported to your doctor. Diabetes can lead to other major foot problems as well, and possibly surgical removal of the toe, foot, or lower leg.
Diabetes can be treated with medication and regular foot exams. It also requires lifestyle changes like quitting smoking, and wearing supportive shoes to mitigate foot trauma.
For more information on foot pain or to schedule an appointment, contact Superior Foot & Ankle Care Center.