Connect With Us
Blogs
Displaying items by tag: ulcers
Poor Circulation Can Cause Big Foot Problems
At Superior Foot & Ankle Care Center, we find that patients may not accurately understand the seriousness of decreased circulation to the lower extremities. The medical condition known as peripheral arterial disease (PAD) describes a situation where plaque (fatty deposits or cholesterol) have adhered to the walls of the arteries that lead to your legs and feet causing a partial or total blockage. This restricts the blood flow to the lower half of your body. PAD is often associated with diabetes and a significant cause of some of the more serious complications of the disease. When oxygen and nutrient-rich blood cannot get to your legs and feet in significant quantities, it makes it difficult to heal wounds and ulcers. This can lead to infection and, in extreme cases, amputation.
Recognize the Symptoms
There is a variety of symptoms of PAD that you may observe or experience. These include:
- Pain or cramping in your feet, legs, thighs or buttocks
- Feeling of coldness in your legs
- Hair loss on your toes and legs
- Bluish or reddish tinge to the skin on your feet or under the toenails
- Thickening and discoloration of your toenails
- Ulcers or wounds on your feet that have not healed after 8-12 weeks
If you notice any of these signs, you should contact our Long Beach office for an appointment by calling: (562) 420-9800. Our podiatrists, Dr. Victoria M. Foley or Dr. Constance Ornelas will want to examine your feet. There are a number of simple, non-invasive tests the foot doctor can perform to see if your symptoms point to PAD.
Reducing Your Risk
In addition to diabetes, PAD is also more common in patients who have high blood pressure, high cholesterol, heart disease or who have suffered a stroke. You are also at a higher risk for developing PAD if you are over the age of 50 or have a family history of PAD, heart disease or stroke. The good news, however, is that some risk factors for PAD are within your control to control. These include:
- Smoking
- Sedentary lifestyle
- Obesity
Making healthy lifestyle choices now and partnering with your podiatrist to monitor your foot health can help you prevent PAD or slow its progression. If you have additional questions about PAD, contact us at our Long Beach office in Douglas Park CA.
6 Tips for Protecting Your Feet with Diabetes
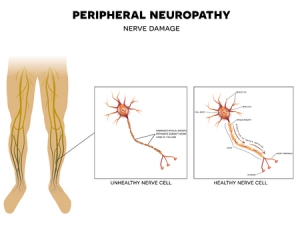
At Superior Foot & Ankle Care Center, we know that diabetes can affect your skin, joints, and bones in a number of ways. Two conditions associated with the disease—peripheral arterial disease (PAD) and neuropathy—are of particular concern when it comes to your lower extremities. PAD is a narrowing or blocking of the arteries to your legs, which can lead to poor circulation. This means that nutrient and oxygen-rich blood necessary for healing cannot reach your legs, feet, and toes as quickly as needed. Neuropathy is nerve damage that can result in loss of feeling in your feet, which makes it difficult to perceive pain and injury. This double whammy means that patients with diabetes are at a higher risk for a host of podiatric problems, including:
- Ulcers and wounds that do not heal properly
- Fungal infections
- Hammertoes
- Ingrown toenails
- Corns and calluses
Difficulty healing can cause even minor foot and toe problems to become major threats with the potential for infection and even amputation. Below are some ways you can be proactive in preventing foot problems if you have diabetes:
- Control your blood sugar. Follow all your doctor’s instructions for managing your diabetes. Watch your diet, take your medications as directed and regularly test to make sure you are on track.
- Schedule regular podiatric checkups. Our podiatrists, Victoria M. Foley or Dr. Constance Ornelas, will work with you to prevent potentially dangerous foot issues. Seeing the foot doctor regularly will increase the chances of catching injuries and infections in their very early and most treatable stages. The podiatrist can also help with nail care, wound debridement and diabetic footwear and orthotics.
- Keep feet clean, warm, and dry. Wash daily and dry thoroughly—especially between your toes. Use a foot powder before putting on socks.
- Make sure shoes fit correctly. Avoid styles that have narrow toe boxes are that are made of very stiff materials. Keep the heel height to 2 inches or less.
- Don’t walk barefoot. This dramatically increases your chances of getting athlete’s foot or a fungal toenail infection, which are contracted by direct contact. You are also more likely to step on a sharp object and injure your foot without shoes.
- Conduct regular self-exams—it’s important that between appointments you are checking your feet and toes daily for any signs of rashes, cuts, blisters, bruises, growths or other indicators that a foot problem is developing. If you can’t see your whole foot as a family member or caregiver to assist you. Contact our Long Beach office immediately by calling (562) 420-9800 if you find anything concerning.
Myths about Hammertoes
At Superior Foot & Ankle Care Center we often find that patients have no trouble identifying a hammertoe—its telltale downward bent at the joint makes it fairly obvious—but often that’s where the knowledge stops. Too often patients suffer for a long time with a hammertoe because they do not fully understand the condition and their treatment options. Below some common myths about hammertoes are dispelled to help patients be more informed about this condition:
MYTH: Hammertoes are caused by shoes that are too tight.
TRUTH: It’s true that improperly fitting shoes can contribute to or exacerbate the condition of hammertoe but usually a muscle/tendon imbalance predisposes the toe to bend downward. In some cases, one toe is longer than the others and pushes up against the front of the shoe. Hammertoe can also be genetic, the result of arthritis or a neurological or structural issue.
MYTH: It’s possible that over time hammertoes will get better without treatment.
TRUTH: Hammertoes are a progressive condition. Although they may progress at varying rates they will not improve and will, in fact, worsen to the point of being disabling if not treated. It’s important to have one of our podiatrists, Dr. Victoria Foley and Dr. Constance Omelas examine your hammertoe to assess how far it has progressed. The foot doctor may order x-rays to get a better look at the current state of the joint and will also want to get a complete medical history. Hammertoes should be monitored by the podiatrist.
MYTH: There’s no real treatment for hammertoes.
TRUTH: Actually there are several conservative options available to the foot doctor to help decrease pain, increase comfort and slow the progression of a hammertoe. These include: strapping or taping the toe to establish realignment, using a custom orthotic device to correct or compensate for a muscle tendon imbalance and doing stretching and other exercises to increase flexibility and strengthen supporting muscles. In addition, patients should choose shoes with low heels that have roomy toe boxes and are made of soft materials to avoid further stress to the toe and irritations such as corns, calluses, and ulcers from developing. If none of these treatments are successful or there are other deformities such as bunions in addition to the hammertoe the foot doctor may recommend surgery to correct the problem.
You have options so don’t suffer needlessly. If you have a hammertoe contact us for an appointment at our Long Beach office today by calling: 562-420-9800.