Connect With Us
Blogs

Arthritis (10)
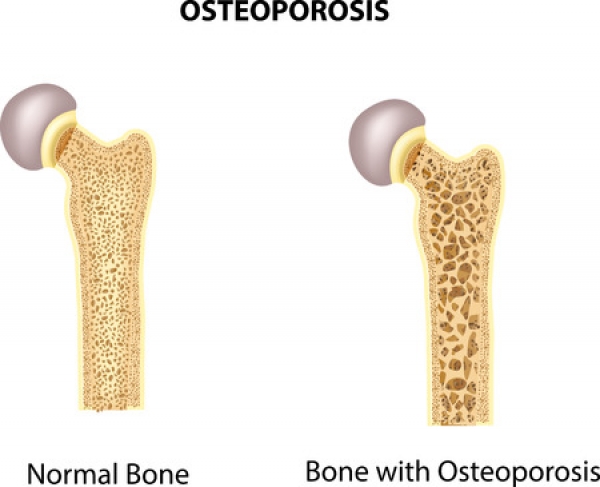
Osteoporosis causes a bone fracture in one out of every two women and one out of every four men over the age of 50. Since May is National Osteoporosis Month, we at Superior Foot & Ankle Care Center think this is a good time to talk about this disease, which can have a big impact on the health of your feet.
Although stress fractures can occur due to trauma, accidents or overuse from an exercise or sport, they can also be the sign of weak bones.
What Causes Osteoporosis
Osteoporosis occurs when you lose too much bone, make too little bone or both. Many patients don’t realize that bone is living tissue that is constantly being torn down and built up. There are many conditions and factors that can result in loss of bone strength. These include:
- Age—your risk increases over the age of 50
- Sex—women have a higher risk, particularly post-menopausal women
- Ethnicity—Latinos, Asian Americans and African Americans are more at risk
- Disease—osteoporosis is often associated with other disease, such as diabetes, lupus and rheumatoid arthritis
- Family history of osteoporosis
If you are experiencing symptoms such as pain, tenderness, swelling, bruising or difficulty bearing weight on the affected foot, it’s important that you not put off getting these symptoms evaluated. Make an appointment at our Long Beach office so that our podiatrists, Dr. Victoria M. Foley or Dr. Constance Ornelas can examine your foot and diagnose the problem and its cause. The foot doctor can help determine your personal risk for osteoporosis and whether or not bone density or other tests should be ordered at this time.
Making Choices for Healthy Bones
Fortunately, there are many ways you can help increase bone strength and lower your risk for fractures, such as:
- Get enough calcium—know how much you should be getting each day and increase your intake of s of yogurt, milk, cheese, leafy greens and other foods that are high in this nutrient. Be sure to also get adequate amounts of vitamin D as this is essential for body to absorb calcium properly.
- Exercise regularly—weight-bearing and muscle strengthening build stronger bones. In general, being active can reduce your risk for decreased bone strength.
- Don’t smoke.
- Fall-proof your home inside and out.
Being educated is your best defense against osteoporosis. Have more questions? Contact us at: (562) 420-9800.
As we age, many of us just accept joint stiffness and pain as an unavoidable part of getting older. But, at Superior Foot & Ankle Care Center, we want to encourage patients to bring those symptoms to our Long Beach office as soon as they start to notice them. Arthritis can be treated, and its progression can be slowed. It’s also important to have our podiatrists, Dr. Victoria M. Foley or Dr. Constance Ornelas examine your feet and properly diagnose your condition because there are multiple kinds of arthritis and they require different treatments.
Signs of Rheumatoid Arthritis
Arthritis is actually a category that contains over 100 different conditions. The two major forms of arthritis, however, are osteoarthritis (the “wear and tear” kind) and rheumatoid arthritis. Rheumatoid arthritis is the most serious of the two. It is actually an autoimmune disorder that causes the body’s immune system to attack its own cells. This leads to an intense inflammatory response within the body. Symptoms may include:
- Joint pain
- Stiffness
- Redness and warmth at the joints
- Swelling
These are also common signs of osteoarthritis. Patients with rheumatoid arthritis may notice additional symptoms, including:
- Fever
- Fatigue
- Symmetry of symptoms—meaning that what is going on in one side of the body is also going on in the other side, i.e., joint pain will occur in both hands or both feet
- Weight loss
- Nerve damage that results in numbness or tingling
- Decreased range of motion
Because rheumatoid arthritis is a systemic condition that can also affect other symptoms in the body, a patient with this disease will need a rheumatologist or other physician to coordinate and mange their care.
Podiatric Help
The foot doctor is part of the care team for a patient with rheumatoid arthritis will help with treatment designed to relieve foot pain caused by the arthritis. Some options may include:
- Steroid injections
- Accommodative shoes
- Orthotics
If you have begun to experience joint discomfort, soreness or pain, it’s important that you make an appointment as soon as possible. Contact us by calling: (562) 420-9800.
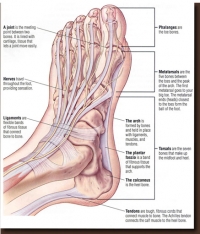
Arthritis is a term that is used to describe over 100 different joint conditions. At Superior Foot & Ankle Care Center we think it’s important for our patients to be informed about arthritic conditions—especially since each of your feet has 33 joints that need to be protected for your foot to function properly.
Although different types of arthritis may have different causes and manifestations, there are some common characteristics. These include:
- Joint pain
- Swelling
- Stiffness
- Limited range of motion
- Redness or heat in a joint
Some of the more common types of arthritis include:
Osteoarthritis—this is the best-known type of arthritis. Also known as “wear and tear” arthritis, it occurs over time as cartilage breaks down with age and use. Osteoarthritis usually comes on gradually and gets worse over time. Being overweight can exacerbate osteoarthritis because of the excess pressure on the joints caused by carrying extra weight.
Rheumatoid arthritis—although rheumatoid arthritis shares the symptom of joint pain with other forms of arthritis, this form of the disease is far more serious in that it is part of a chronic inflammatory system of diseases that can affect various systems of the body including lungs, heart, eyes and nervous system.
Traumatic arthritis—an injury or trauma to a joint such as a bad sprain, fracture or being hit with a heavy object can damage cartilage and lead to arthritis.
Gout—this form of arthritis occurs when uric acid builds up in the joint and then crystallizes, causing severe pain, inflammation and swelling. Gout most often affects the big toe joint and can be triggered by certain foods, such as shellfish, red meat, organ meats, red wine, brandy, and other alcoholic beverages.
Psoriatic arthritis—in some people with the skin condition of psoriasis a form of arthritis may develop as well. Arthritis may be mild and tends to get worse when the skin condition worsens.
With any form of arthritis, early detection and treatment is key to slowing the progression of the disease and managing the symptoms. If you have any signs of joint disease, it’s important that you contact our Long Beach office (562-420-9800) as soon as possible so that one of our podiatrists, Dr. Victoria Foley or Dr. Constance Ornelas can determine the source of your joint discomfort along with the appropriate treatment.
World Arthritis Day takes place in October and here at Superior Foot & Ankle Care Center, we’d like to take this opportunity to explore the relationship between food and joint health. Overall, we know that maintaining an appropriate weight greatly reduces the strain on your joints (and the rest of your feet), lowering your risk for arthritis and other foot problems. Below are some foods to choose or stay away from if you suffer from arthritis or other joint conditions:
Eat These:
Fish high in omega-3 fatty acids. These include salmon, sardines, tuna, anchovies, scallops and other cold-water fish. Omega 3’s have inflammation-fighting properties and research has shown that people who consume the highest amounts of them have the lowest levels of two inflammatory proteins in their bodies. If you can’t stand fish, take a fish oil supplement. A recent study found that 600-1,000 mg per day could ease joint swelling and pain and reduce the duration of morning stiffness in rheumatoid arthritis sufferers.
Fruits and Vegetables. Eating a rainbow of produce will give you many nutrients and antioxidants. Among the heavy hitters for reducing inflammation are: citrus fruits, red and purple fruits such as blueberries, strawberries and cherries and dark greens like spinach, kale and broccoli.
Good oils. Of course, all oil should be used in moderation but 2-3 tablespoons of olive oil a day can help reduce joint pain because it contains a compound that has properties similar to that of nonsteroidal, anti-inflammatory medications. Other “good oils” include safflower and avocado oil and also walnut oil which is high in omega 3’s.
Skip These:
Sugar. Foods with processed sugars (cakes, cookies, candy bars, sodas and fruit juices) release messengers called cytokines that actually create an inflammatory response in the body. Read labels because sugar has many names. Anything ending in “ose” is usually a sugar.
Saturated and Trans Fats. These trigger fat tissue inflammation which not only worsens arthritis but is an indicator of heart disease too.
Mono-sodium glutamate (MSG). Although most often found in prepared Asian foods and soy sauce, MSG is also added to many fast foods, soup mixes, salad dressings and deli meats. MSG opens 2 pathways to chronic inflammation.
Food is just one way to help control arthritis. If you are experiencing pain, stiffness and/or swelling of the joints in your feet and ankles, contact our Long Beach office by calling: (562) 420-9800. Our podiatrists, Dr. Victoria Foley or Dr. Constance Omelas will examine your feet and help develop a plan to best deal with your joint issues.
Did you know that the term arthritis refers to over 100 joint diseases and disorders? At Superior Foot & Ankle Center we want to pass on some information about this group of diseases that currently affects 1 in 5 adults in our country and approximately 300,000 babies, children and teenagers. Generally speaking, the risk of arthritis increases with age and more women than men are affected by these diseases. Your feet and ankles are prime targets for joint disorders, with 33 joints per foot. Common symptoms of arthritis include: pain, swelling and stiffness in joints, which limits range of motion and makes it difficult to move. There are 4 main categories of arthritis:
Degenerative—known as osteoarthritis, this is the most common type of arthritis. It occurs as a result of cartilage break down which can occur as we age. With decreased cartilage bone rubs against bone causing pain and stiffness. Factors that increase your risk for osteoarthritis include: being overweight, previous injury and family history.
Inflammatory—this type of arthritis is related to a dysfunctional immune system that attacks the joints with inflammation. Two examples in this category are rheumatoid arthritis and psoriatic arthritis. These conditions are more complex and affect other systems in your body besides your joints.
Infectious—in some cases joint inflammation can be caused by the invasion of a bacterium, virus or fungus into the joint. Conditions such as salmonella or food poisoning, hepatitis C and certain sexually transmitted disease like Chlamydia and gonorrhea can cause this type of arthritis. If caught in the early stages, antibiotics may be able to eliminate the joint infection but chronic arthritis is a possible outcome.
Metabolic—this refers to gout, a form of arthritis that frequently strikes the joint at the base of the big toe. It has to do with the body being unable to rid itself of uric acid. An overabundant amount of this substance will cause crystals in the joints and sudden and extreme pain.
If you have noticed pain or discomfort in the joints of your feet or ankles, make an appointment at our Long Beach office by calling: (562) 420-9800 so one of our podiatrists, Dr. Victoria Foley or Dr. Constance Omelas can evaluate your feet and determine if you are suffering from an arthritic condition.
You may have heard one of the many myths surrounding broken toes: that it will heal on its own, or that it’s okay as long as you can still walk on it. While reassuring, these common misconceptions are entirely false, and can have potentially severe consequences. Leaving a broken toe untreated can result in various complications, from misaligned bones and infection to arthritis and permanent foot pain. The thought of a doctor visit or hospital bill may make you cringe at first, but your feet will thank you for it in the long run.
Here is a look at the signs that your toe is broken, the dangers of avoiding treatment, and the steps you need to take to make sure your toe heals properly.
Signs Your Toe Is Broken
Even the smallest of accidents can result in toe trauma: dropping an object on the foot or stubbing your toe are common misfortunes that often lead to injury. Moreover, repetitive trauma to the toe over time can result in a stress fracture. While it’s tempting to try to tough it out, it’s important to listen to your pain to identify whether or not your toe is fractured.
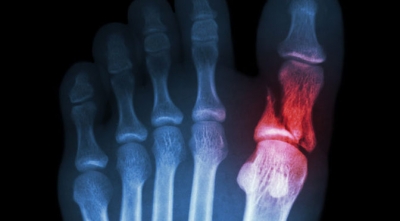
It usually requires significant force to break a bone, although a little less so for the toes since their bones are so small. Regardless, the instance of fracture will be extremely painful. The toe will begin to swell as the fractured bone bleeds, resulting in bruising as the blood reaches the skin. You may also see blood pool beneath the toenail. In many cases an injury to the toe also involves damage to the toenail, which further increases your risk of infection should the toenail expose the tissue underneath. The fracture usually makes it extremely painful to walk, although this is not always the case. Even if you can still manage to walk on the toe, that doesn’t eliminate the possibility of a fracture.
Seek prompt medical attention if your toe shows signs of:
- Swelling
- Pain
- Bruising, or blue or gray spots surrounding the site of trauma
- Stiffness
- Trouble Walking
- Deformity
- Infection
- Bleeding, especially beneath the toenail
- Coldness, numbness, or a tingling sensation indicative of nerve damage
Complications of an Untreated Broken Toe
Leaving a broken toe untreated can have serious and long term complications, including, but not limited to:
- Infection: If the injury has left an open wound, or especially if there is damage to the toenail, you are at risk of contracting an infection. Any exposure of a broken bone can lead to a bone infection (osteomyelitis), which is usually caused by the bacteria staphylococcus aureus. Once diagnosed, your doctor may implement antibiotics straight into the bloodstream intravenously, or you may need to take medication for up to six weeks. If the infection is severe, your doctor may have to perform surgery to remove the infected bone.
- Compound fracture: A compound fracture is when a broken bone penetrates the skin, leaving the bone vulnerable to infection.
- Deformity: An untreated broken toe has a high likelihood of healing incompletely or improperly, potentially resulting in crookedness or deformity which may require corrective surgery down the road.
- Osteoarthritis: An improperly healed fracture can lead to a future of osteoarthritis as you age, generalized foot pain and discomfort, as well as an increased likelihood of further foot injury.
Toe Fracture Diagnosis and Treatment
Your podiatrist will order an X-ray to confirm a toe fracture. Once properly diagnosed, a mild toe fracture can be treated at home under the guidance of your trusted podiatrist. Home treatment essentials include elevating the foot above the level of the heart in order to decrease swelling, icing the injury for 20 minutes every 2 hours for the first 2 days, and of course rest and crutches to avoid bearing weight on the injury while you recover. OTC acetaminophen or ibuprofen should be sufficient for coping with the pain, although your doctor may prescribe a stronger medication if your fracture is severe.
If the fracture is minor or located in one of the small toes, your doctor may simply implement buddy taping, which involves taping the damaged toe to its neighbor for support while it heals. In cases where the toe fracture becomes rotated or displaced, the doctor will need to perform a reduction. This involves administering a shot of local anesthesia before realigning the toe back into its proper position.
Casting may be required in more severe fractures: where the big toe is injured, the joint is damaged, the injury involves various small toe fractures at once, or if a bone in the foot is injured in addition to the fractured toe. When wearing a cast, a sturdy shoe should be worn to provide maximum comfort and support. If all goes well, the fracture should take up to six weeks to heal.
Schedule a Consultation with Dr. Vikki and Dr. Connie
If you have suffered injury to your feet, toes, or ankles, don’t wait for complications to arise.Schedule a consultation with trusted podiatrists Dr. Vikki and Dr. Connie at the Superior Foot & Ankle Care Center today.
How Aging Contributes to Foot Issues
Over time, our bodies begin to wear down and our feet are no exception. Myriad changes occur to our feet as we reach our senior years. This includes muscular and skeletal changes, as well as skin and toenail changes, each coming with their own possible challenges. Here is an overview of some of the common foot issues that can come with age:
Changes in Size
Most would assume that shoe sizes stay the same after puberty, but this is not the case. As we age our feet “spread,” which may alter the size of the shoe you should be wearing. Every time you go shopping for a new pair of shoes, you should measure your feet, both for length and width. If it seems like your shoes are growing less comfortable day by day, then you might want to make sure you aren’t outgrowing them.
Skin Issues
One of the more obvious changes we undergo as we age is the thinning of skin. Our feet are no different; and since they are an area that is often subjected to frequent friction, they can see a lot of complications. Due to the weakening and drying of the skin, abrasions are common. Make sure to use moisturizer to keep your skin supple and soft.
Several types of keratosis can make your feet skin look as if it is cancerous or infected, but these raised pigmented bumps are usually benign. Any changes in your skin should be addressed by a physician, as some of these conditions may be masking a more serious affliction.
Arthritis
As the wear and tear on our joints adds up over time, arthritis begins to set in. Arthritis of the feet can be one of the most painful and debilitating forms of this condition, since the feet bear the weight of our bodies. Reduced bone density can also play a role in this type of joint pain.
The weakening of joints and bones can also lead to more frequent fractures and sprains, so it’s important to wear durable, supportive, and comfortable shoes.
Swelling
Circulation problems are also more common with age. Issues with the veins in the legs can cause feet to swell, making shoes ill-fitting from day to day. Sometimes only a single foot will swell, other times both will. Hormonal changes and some medications can be the cause of these issues, as well.
Bunions
An additional reason to wear shoes that fit correctly is bunions. Wearing narrow shoes can cause your big toes to press inwards, jutting out the joint and causing it to elongate and press on the skin. Bunions aren’t only caused by wearing small shoes, as there is also a genetic component to their formation. They can also form on your smaller toes, but they are more pronounced on the big toes.
Hammer Toes
Ill-fitting shoes and arthritis can also cause a condition known as hammer toe. Normally, our toes point outwards from our body, but a hammertoe causes them to point downwards towards the ground. This can affect any toe on the foot, and be quite painful. The physical cause of this downward turn is a dislocation of the middle joint in the toe. Dislocation can be caused by wearing tight shoes such as high heels; or factors such as injury, arthritis, or pressure from the aforementioned bunions.
Gout
A specific type of arthritis, gout is caused by having too much uric acid in the blood stream. While this doesn’t cause symptoms in all patients, in certain individuals these high levels of uric acid cause crystals to form on the joints, usually the big toe. Gout manifests in sudden attacks of pain in the big toe until it is treated. Risk factors for gout include being overweight and having a diet high in meat and alcohol.
Gout is usually somewhat obvious by its visible effects on the big toe, causing swelling and redness. Steroids can stop a sudden gout attack, and there are long-term treatment options as well for chronic gout.
Schedule a Consultation with Dr. Vikki and Dr. Connie
As with any part of the body, investing in your foot health is essential to ensure that your feet age gracefully alongside you. To keep your feet fit for years to come, schedule a consultation with trusted podiatrists Dr. Vikki and Dr. Connie today at the Superior Foot & Ankle Care Center.
What Could Be Causing Your Heel Pain?
Do you ever find yourself walking on your toes because it’s too painful to plant your heel? Has your heel been sore for a while, but you just aren’t sure what’s causing the pain? Here’s a quick look at some of the causes of heel pain, why they occur, and how to treat them.
The Most Common Causes of Heel Pain
The most common causes of heel pain are Achilles tendinitis (back of the heel) and plantar fasciitis (bottom of the heel).
- Achilles tendinitis is an injury caused by the overuse of the Achilles tendon (the band of tissue that connects the calf muscle at the back of the lower leg to your heel bone). Achilles tendinitis is caused by repetitive or intense strain on the Achilles tendon; but the structure of the Achilles tendon also weakens with age, making it more susceptible to injury.
Symptoms: The associated pain usually begins as a mild ache in the back of the leg or above the heel after running or other sports activities. More severe pain may occur after prolonged running, stair climbing, or sprinting.
Treatment: Achilles tendinitis usually responds well to self-care measures. However, if your symptoms are severe or persistent, your doctor may suggest other treatment options, such as: over-the-counter pain medications, physical therapy exercises, orthotic devices, or surgery. - Plantar fasciitis commonly causes a stabbing pain that usually occurs with your very first steps in the morning. The pain usually decreases once your foot limbers up, but may return after long periods of standing or sitting. Plantar fasciitis is common in runners, people who are overweight, and those who wear unsupportive shoes.
Symptoms: Pain and inflammation of the thick band of tissue that runs across the bottom of your foot, connecting your heel bone to your toes.
Treatment: Most people can recover with conservative treatments after a few months. In some cases, your doctor may recommend other treatments, such as: pain medications, physical therapy, night splints, orthotics, steroid shots, stem cell injections, or surgery.
Other Causes of Heel Pain
Some less common causes of heel pain include:
- Bursitis is a painful condition that occurs when the bursae (small fluid-filled sacs that cushion the bones, tendons, and muscles near joints) are inflamed.
Symptoms: When the affected joint feels achy or stiff, hurts more when you move it or press on it, or looks swollen and red.
Treatment: Involves conservative measures (rest, ice, and pain relievers). Other treatment options include: medication, therapy, injections, assistive devices, and surgery. - Osteomyelitis is a bone infection that usually affects the feet of people who have diabetes.
Symptoms: Fever or chills; irritability or lethargy (in young children); pain in the infected area; and swelling, warmth, and redness over the infected area.
Treatment: The most common treatment is surgery, followed by antibiotics. Depending on the severity of the infection, surgery may include: draining of the infected area, removing diseased bone and tissue, restoring blood flow to the bone, removing any foreign objects, or amputating the limb. - Peripheral neuropathy is the result of damage to your peripheral nerves that can often cause weakness, numbness, and pain. It can be caused by traumatic injuries, injections, metabolic problems, inherited causes, and exposure to toxins.
Symptoms: Numbness, prickling, or tingling; sharp, jabbing, throbbing, freezing, or burning pain; extreme sensitivity to touch; lack of coordination and falling; and muscle weakness or paralysis.
Treatment: Medications (pain relievers, anti-seizure medications, topical treatments, and antidepressants), therapies (transcutaneous electrical nerve stimulation, plasma exchange and intravenous immune globulin, physical therapy, and surgery), or alternative medicine (acupuncture, alpha-lipoic acid, herbs, and amino acids). - Reactive arthritis is joint pain and swelling triggered by an infection in another part of your body (usually the intestines, genitals, or urinary tract).
Symptoms: Pain, stiffness, eye inflammation, urinary problems, and swollen toes or fingers.
Treatment: Physical therapy or medications, such as: nonsteroidal anti-inflammatory drugs, corticosteroids, or rheumatoid arthritis drugs. - Stress fractures are tiny cracks in a bone that are caused by the repetitive application of force (jumping up and down or running long distances).
Symptoms: Mild or severe pain that worsens over time, and swelling.
Treatment: Reduce bone’s weight-bearing load until the fractures are healed. You may need to wear a walking boot, brace, or use crutches. Surgery may be required, although that is not common.
Contact Your Doctor
The first step to knowing what is causing your heel pain is to consult with an experienced doctor, so that you can get a proper diagnosis. Be sure to consult with Dr. Vikki and Dr/ Connie today. With years of collective experience in their fields, they will be able to help you get to the bottom of your foot pain.
How to Treat Bone Spurs
Have you been experiencing a sharp pain in your foot, but you can’t figure out why? Chances are that you have developed a condition called bone spurs.
A bone spur is a small bony growth or a collection of growths which form on joints like the spine, shoulders, hands, hips, knees, and the feet. While we will be focusing on the feet, much of the information below will apply to bone spur treatment in general:
Bone Spurs: Causes
A bone spur occurs when the body attempts to repair itself by building extra bone on areas affected by long periods of pressure, rubbing, or stress.
Bone spurs rarely cause pain on their own. If they grow on the feet, however, calluses may form to cushion the affected area. As the wear and tear on the joints continue, the spurs may compress the surrounding ligaments, tendons, or nerves. This results in injury to the surrounding tissue, in addition to swelling, pain, and tearing.
There are several factors which may contribute to a bone spur. The aging process is partly to blame: cartilage, which covers the ends of bones in a joint, slowly wears away due to a process called osteoarthritis. The damage to the joints will lead to pain and swelling, and will often result in a bone spur. Osteoarthritis is a common cause of bone spurs in joints of the feet and spine.
Tight ligaments will also make you more vulnerable to bone spurs. Many factors can cause this tightness, including strenuous activities which affect the feet like dancing, running, long periods of walking, basketball, and tennis. Other factors include:
- Obesity: excess weight will result in excess pressure on the feet.
- Tight-fitting shoes (like high-heels) can put undue pressure on the feet, causing stress and tightness in the foot, particularly in the heel. Shoes which lack proper arch support, like worn-out shoes, can worsen this problem as well.
- Plantar fasciitis, an inflammation of the plantar fascia ligament. Repeated stretching and tearing of the plantar fascia and other muscles in the feet can lead to increased wear and tear on the heel.
- Abnormalities in walking.
- Diabetes.
- Occupations which require long periods of standing.
- Flat feet or high arches.
Bone Spurs: Treatment
Bone spurs rarely require treatment, unless they cause frequent pain or damage to surrounding tissues. Unless these symptoms are present, it is difficult to detect a bone spur without an X-ray (though it is rare to use an X-ray for this condition, since it rarely causes symptoms). Since heel spurs and plantar fasciitis are closely related, many of the same treatment methods for plantar fasciitis will be used for bone spurs as well. Consider these tips to find relief:
- Resting from the activity causing the bone spur will be recommended. If it cannot be avoided (due to an occupation, for example), ice the affected area immediately after the activity is finished.
- If you have a heel spur, warming up before a strenuous activity and stretching the calf muscles may also be helpful. These stretches will gently lengthen the calf muscle, relaxing the tissue surrounding the heel. Commit to stretching several times throughout the day, particularly in the morning and after a prolonged period of sitting or standing, when the muscles in the feet are stiffest.
- If osteoarthritis or plantar fasciitis are causing pain or damage, weight loss will reduce pressure on the joints and mitigate symptoms.
- Learn how to take proper care of your joints.
- Visit a physical therapist to have an ultrasound or deep tissue massage, especially if your pain is related to plantar fasciitis.
- Wear shoes with good arch and heel support. Try using an orthotic insert in your shoe, to add more support or padding for a corn or callus.
- A doctor may prescribe a corticosteroid injection to reduce pain and inflammation. This will be more of a last resort, since side effects may exacerbate symptoms, especially with heel spurs.
- Discuss surgical removal of the bone spur, which will loosen the plantar fascia.
Consult the Experts
Bone spurs are difficult to detect, and the volume of potential variables related to foot pain can make it difficult to determine the cause. If you’re suffering from foot pain, schedule your consultation with expert podiatrist Dr. Vikki today. Dr. Vikki has a reputed record of patient satisfaction, and is the trusted podiatrist of Special Olympic athletes.
For this and all related foot care concerns, the caring professionals at Superior Foot & Ankle Care Center are happy to help with your podiatric needs.
There are many physical and psychological health benefits related to foot massages. Daily foot massages, for a couple minutes at a time, has been proven to fight depression and relieve headaches. Here is a list of the many health benefits of having regular foot massages.
Stress Relief
Regular foot massages have been shown to greatly relieve stress, as well as, many of the symptoms associated with it, such as energy loss and headache. A five to ten-minute foot massage, after a long day, can significantly relieve fatigue and increase feelings of well-being. Try using scented oil when administering your foot massage, for the added benefit of aromatherapy.
Blood Circulation & Sleep
Poor blood circulation causes many foot health issues. Regular foot massages can regulate your blood flow and keep your feet healthy, as well as, combat foot health problems such as inflammation, swelling, and pain. Foot massages also stimulate the limbic system and help prevent varicose veins. When night falls, massaging your feet right before bed helps you unwind, relax your nerves, and relieve any aches and pains-promoting restful sleep. Try using a lavender scented oil when administering your foot massage, as the lavender scent in calming and promotes relaxation.
Foot Health
Not only does regular foot massage promote healthy blood circulation, it can also relieve everything from minor aches to arthritis pain. In addition, it has been shown that regular foot massages, with olive or coconut oil, can significantly relieve the pain associated with foot tendonitis. Additionally, daily foot massage can help strengthen your ankles and increase your flexibility, which can prevent foot-related injuries.
Pain & Depression
While it’s well known that foot massages relieve foot pain, it also an effective way to treat other common body aches and pains. For example, regularly massaging your ankle and Achilles tendon can help relieve lower back pain and pressure. Additionally, because foot massage is such an effective stress relief treatment, it has also been shown to relieve migraine and headache pain. Regular foot massages also help you feel relaxed and balanced, promoting a sense of calm. Considering stress, tension and fatigue are associated with situational depression, daily foot massages have been shown to not only combat to these symptoms, but depression itself.
Other Health Benefits
- Helps manage PMS and Menopause symptoms.
- Assists those suffering from restless leg syndrome manage their illness.
- Relieves swollen feet during pregnancy.
- Relieves the chronic pains of arthritis in the feet and legs.
- Helps those with minor foot injuries to heal quicker.
Now that you are aware of the health benefits from regular foot massages, be sure to incorporate this into your daily routine, along with your regular visits to Superior Foot & Ankle Care Center. If you have any questions or concerns about your foot health, please feel free contact us today, at 562-420-9800.