Connect With Us
Blogs
Blog
Children categories
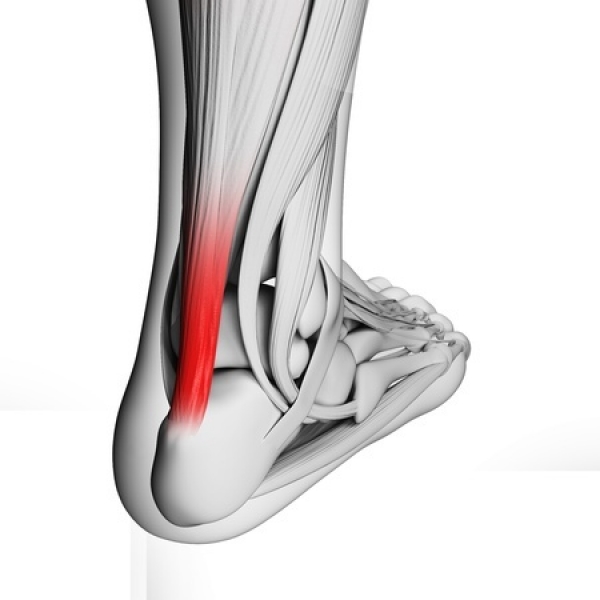
The day after a particularly intense workout or a long run you may notice pain ranging from mild to extreme in the lower part of the back of your leg. Or, you may be noticing a sluggish feeling in your leg accompanied by stiffness and/or a dull ache that lessens as you stretch the leg and get going with your day. All of these are possible symptoms of Achilles tendonitis—an inflammation of the large tendon that runs between the bottom of your calf muscle and your heel that we see often at Superior Foot & Ankle Center.
Tendonitis is primarily caused by overuse or trauma to the tendon. Scenarios that can result in inflammation and injury to the Achilles tendon include:
- Suddenly increasing the distance or intensity of your run or workout
- Doing too much too soon in a new exercise routine or starting up after a period of inactivity
- Overpronation
- Inappropriate footwear choices
- Not stretching enough before sports or exercise
- A trauma to the tendon caused by a sudden or wrenching movement (like taking off for a sprint)
- Heel bone deformity
- Age related wear and tear
Treatment and Prevention
Mild cases of Achilles tendonitis can be resolved by resting the leg and avoiding activities that put stress on the tendon. If the pain is persistent however, and doesn’t seem to improve with rest, it’s time for an appointment with one of our podiatrists, Dr. Victoria Foley or Dr. Constance Omelas. The foot doctor can evaluate just how severe the tendonitis is and make recommendations for relief. These may include: icing, specific stretching exercises to do before and after exercise and a heel cup or other orthotic device to help prevent overpronation and increase arch support. Wearing properly fitting shoes that are designed for the sport or activity you do and following a sound program that increases in intensity gradually can help prevent inflammation the Achilles tendon.
To learn more about how to prevent or treat Achilles tendonitis, call our Long Beach office at: (562) 420-9800.
Among the more common injuries we see at Superior Foot & Ankle Care Center are ankle sprains. In many instances these injuries come about on the playing field in soccer or football, for example, when your foot is planted and headed one way and then suddenly gets twisted in a different direction. Ankle sprains can also occur less dramatically, like stepping off a curb or missing the bottom step.
How Severe is the Sprain?
If you’ve sprained your ankle you will most likely experience pain, swelling and bruising. Ankle sprains can range from mild to severe. The degree of pain and swelling will correlate to the severity of the sprain. If you have sprained your ankle badly, you may not be able to bear weight or walk on it. Getting your ankle evaluated promptly and beginning rehabilitation as soon as possible is very important. Patients who delay treatment or just limp along at home until their ankle stops hurting are more likely to have repeated sprains and possibly long-term, chronic ankle pain and weakness.
Repairing the Damage
If you have swelling and bruising along with pain after twisting your ankle it should be evaluated by one of our board certified foot and ankle surgeons, Dr. Victoria Foley or Dr. Constance Omelas. After examining your ankle, the foot doctor will most likely want you to have a digital x-ray (which can be done conveniently right in our Long Beach office) to rule out a fracture, which can happen at the same time as a sprain. Once the podiatrist has assessed the degree of injury, an appropriate treatment plan can be developed.
The PRINCE Regimen
Until your appointment, you can care for your ankle using the PRINCE regimen:
Protection: Use a brace or other ankle support
Rest: Stay off your foot or avoid bearing weight by using crutches
Ice: Apply ice for 10-20 minutes every hour or two for the first 24 to 72 hours
Nonsteroidal anti-inflammatory medications: Ibuprofen or acetaminophen for pain relief
Compression: An ACE bandage or elastic compression wrap for the first 24-36 hours will help reduce swelling
Elevation: Keep your ankle above the level of your heart for 2-3 hours a day if possible
To get your ankle checked, contact us at: 562-420-9800 as soon as possible after the injury occurs.
According to the American Podiatric Medical Association, most Americans will have put 75,000 miles on their feet by the time they reach the age of 50! Although in some ways our lives have become more sedentary than in previous generations we now engage in much more rigorous fitness activities to compensate then in times past which can mean even greater wear and tear on feet and ankles. Take running, for example, which puts pressure on each foot equivalent to 3 to 4 times the weight of your body. Even walking for a person who weighs 150 pounds will exert an estimated 127,000 pounds of pressure per foot per mile. At Superior Foot & Ankle Care Center we want to share these figures to help you gain more respect for your feet and the importance of caring for them. Your feet are wonderfully made complex structures comprised of 26 bones, 33 joints and more than 100 muscles, tendons and ligaments. You can help keep your feet healthy and prevent many common problems by following a few footcare basics:
- Develop a regular care regimen. Wash feet daily and dry thoroughly (especially between the toes). Apply a rich moisturizer to keep skin supple and hydrated. If you tend to sweat excessively, use a talc or anti-fungal foot powder as well.
- Make good shoe choices. Poorly fitting shoes are one of the biggest causes of foot problems. Be sure that toes are not squeezed and that the shoes you wear provide good arch and ankle support. Avoid overly high heels and discard shoes when they are worn out.
- Exercise wisely. Being fit is important for your feet and the rest of your body too. Regular exercise is recommended but be sure to start gradually and work up to longer and more intense workouts in order to avoid injury.
- Inspect your feet periodically. Look for changes in size, shape, skin color or temperature as well as any lumps, bumps or unusual changes in your toes. Most foot problems are more successfully treated and with less invasive means if caught in the early stages. Report anything suspicious to your foot doctor.
- Don’t ignore pain in your feet—it’s never normal! Our board certified podiatrists, Dr. Victoria Foley and Dr. Constance Omelas will conduct a thorough examination of your feet and diagnose the source of your pain. A custom treatment plan will soon have you on track to getting back to the active lifestyle you normally enjoy. Contact our Long Beach office by calling: 562-420-9800 for an appointment.
Do you ever have those mornings when you’re in a rush, so you don’t have all the time you need to properly perform your skin care regimen? On one of those mornings have you ever secretly used your hand or foot skin cream on your face?
You probably think “What’s the harm?” Here’s a look at why all skin creams aren’t the same and what you should be using to treat dry feet.
Skin Cream: Is Each One Equal When It Comes to Your Feet?
The simple answer is no, not all skin creams are created equal because each skin cream is designed to treat specific areas of the body. By their nature, the skin of your face and that of your hands or feet aren’t the same. The skin on your face is more delicate, while the skin on your hands and feet is thicker. Skin is actually different everywhere, which means different care and different formulas.
Hand and foot creams may have the same basis as face creams, and they have ingredients in common, but they have different concentrations of them, which is what makes all the difference.
Hand and foot creams need to work as barriers. For this, they need to have high concentrations of wax, greases, oils, and chemical exfoliating agents. If you use them on your face, you risk causing blocked pores and pimples. So, while you can use a face skin cream on your feet or your hands, you shouldn’t do it the other way around—even if you have a tiny dry patch. Foot and hand creams are just too rich, thick, and sticky to be applied to your facial skin.
Treating Dry, Cracked Feet at Home
With the cold weather just over the horizon, so too are dry feet. Here are some tips on how you can treat dry, cracked feet at home:
- Wash feet daily with warm, soapy water. Don’t use hot water because it dries out skin. Hot water is also harmful to diabetics and anyone else with impaired circulation to the feet.
- Exfoliate the feet, especially the heels, while washing. Use a warm cloth or pumice stone, and rub the skin gently to slough off dead skin.
- Dry feet thoroughly. Dry well between the toes since fungus and bacteria like to grow in warm, moist, dark places.
- Moisturize daily. Try using products containing urea, which is naturally present in skin cells. Using a product that has urea increases the skin’s ability to hold in moisture. Avoid moisturizer between the toes. Put on cotton socks after moisturizing.
- Soak your feet. Limit foot soaks to 10-15 minutes, three times a week. Soaking for long periods of time can dry out your feet. Use a solution of ¼ cup white vinegar and enough warm water to cover the feet up to the ankles. The mild acetic acid in vinegar softens skin.
Making Your Own Moisturizer
Here are some easy home-made moisturizers that can help heal dry, cracked feet.
Coconut Shea Butter—combine ¾ cup coconut oil with ½ cup shea butter in a sauce pan and place on low heat. Once they’ve melted, remove from the heat and stir in 15 drops of lavender essential oil. Store in a glass jar with a lid somewhere cool. Massage this foot moisturizer into feet, focusing on dry, cracked areas. Cover feet with cotton socks right away. Try this once in a while for some nice pampering or repeat on a regular basis to soften dry feet.
Honey Foot Cream—warm 1 cup of organic honey slightly to make it easier to spread. Stir in 2 tablespoons of warm milk and the juice of ½ an orange. Use a pumice stone or foot file to slough off some of the callused skin before spreading a layer of mixture evenly onto your heels, massaging as you go to help it sink in. Leave it on for 45 minutes and then rinse with warm water and dry thoroughly. Do this twice daily. If you prefer, you can apply this skin cream before bed and let it dry and then leave it on overnight.
Treating Dry Feet
If you are concerned about having dry feet or have any questions about what products are safe to use on your feet, then you should book an appointment with Dr. Vikki and Dr. Connie of the Superior Foot and Ankle Care Center. With years of collective experience in their field, they will be able to help you find the best products to use on your feet.
If you’ve noticed that your toes have been looking a little strange to you lately, or that they have become unusually rigid and tight, you may have hammertoes. A hammertoe is as unpleasant as it sounds: as the namesake suggests, a hammertoe is a deformity which causes the toes to bend sharply downwards rather than straightforward, resembling the silhouette of a hammer.
It is a common but painful condition affecting over 200,000 Americans per year, typically resulting from years of wearing ill-fitting shoes with narrow toe boxes, such as fashionable heels. Fortunately, hammertoe is easily diagnosed and treated, if you know what to look out for. Here is a look at hammertoe causes, symptoms, and treatment:
What Is Hammertoe?
While hammertoe can affect any of the toes, it is most commonly seen afflicting the second, third, or fourth toe. This deformity results when the middle joint of the toe becomes dislocated, forcing the toe to bend sharply downward and buckle in this position. The underlying cause is a muscle and ligament imbalance surrounding the toe joint, where the muscles have tightened from being forced into a flexed position – such as when wearing cramped shoes – to the point where they can no longer straighten out. Pain can result from excessive friction and rubbing against the top of the deformed toe, and corns and calluses may form to further exacerbate the condition.
A number of factors can contribute to the development of hammertoe:
- An uncommonly high foot arch
- Flat feet
- Cramped or ill-fitting shoes
- Pressure from a bunion
- Toe injury
- Arthritis
- Tight tendons or ligaments in the feet
Symptoms & Diagnosis of Hammertoes
Hammertoe is easily recognizable, but you’ll want to confirm with a podiatrist for an official diagnosis. Common symptoms which indicate hammertoe include:
- Pain when walking
- Pain when stretching the affected toe
- A toe which bends downwards and is difficult to move
- Difficulty wiggling the toes or flexing the foot
- Calluses or corns
- Toes taking on a claw-like appearance
There are two types, or stages, of hammertoes: flexible and rigid. A flexible hammertoe means that the condition was caught within its early stages, where the toe is still able to move at the middle joint. This form of hammertoe is still mild, and has a number of various treatment options available. When the condition progresses to the point where the tendons become rigid enough to push the joints out of alignment, the toe will become immovable. At this stage, surgery is usually required.
Your podiatrist can often visually diagnose hammertoe with a physical exam. However, if you’ve had a toe injury, imaging tests may also be required.
Hammertoe Treatment & Prevention
The course of treatment depends upon how far your hammertoe has progressed.
Mild hammertoe that has been caught in its early stages and still remains flexible has a much greater variety of treatment options available. The first step is identifying the cause responsible for the hammertoe. If cramped footwear is the issue, simply switching to better shoes can remedy the condition. If flat feet or high arches are to blame, custom insoles or toe pads can offset the damage. For corns, over-the-counter medications or pads may suffice. Again, consult a podiatrist to determine the source of your hammertoe, to properly advise you on the appropriate treatment option.
Severe hammertoe that has become rigid and inflexible will require surgical intervention to restore motion to the toe. Hammertoe surgery may involve repositioning of the toe, removal of damaged bone, and realignment of the tendons.
The best prevention tip for hammertoes is to make sure that your shoes are fitting properly, and that your feet’s special needs are met. This means getting insoles or orthotics if you require them, and ensuring that your shoes are not too snug nor the heels too high. In general, it is recommended to avoid any heel over 2 inches in height. If you notice any pain, discomfort, or deformity, consult a podiatrist at your earliest convenience to avoid further complications.
Schedule a Consultation with Dr. Vikki and Dr. Connie
If walking has become painful and you suspect that hammertoes are to blame, schedule a consultation with trusted podiatrists Dr. Vikki and Dr. Connie at the Superior Foot & Ankle Care Center today.
A trivia question: What is the best exercise for your feet? (The answer can be found at the end of this article.)
The likes of Stephen Hawking, Theodore Roosevelt, and Abraham Lincoln have all employed the feet metaphor in some of their most inspiring quotes, underscoring the literal and figurative significance of paying attention to our feet. And yet, so many of forget to do so. This is a shame, as our feet are more fascinating than most of us realize.
Fun Feet Facts
The University of California, Berkeley, has a list of facts about our feet that are worth our time knowing about – not just for the sake of curiosity, but even to better inform how we look after our feet:
- Each foot contains 26 bones (with both feet together having more than one quarter of the body’s total bones); 33 joints; and more than 100 tendons, ligaments, and muscles.
- There are more than 100,000 nerve endings in each foot, which provide sensory feedback to your brain, enabling you to automatically adjust your gait according to your environment to reduce impact forces on your body. Wearing shoes alters this feedback mechanism.
- Each foot has about 125,000 sweat glands, which combined excrete more than a cup of perspiration a day (no wonder feet sometimes don’t smell so good).
- A person who averages 8,000 to 10,000 steps a day (the minimum recommendation for overall good health) will, over a 75-year lifetime, walk the equivalent of circling the world three times.
- During high-impact activity, the forces on your feet can be equal to twice your body weight—or even more.
Additional Bonus Facts
- Toenails take longer to grow than fingernails do. It takes approximately a year and a half to grow an entire toenail. In addition, research shows that being younger, male, and/or a nail biter could all be driving factors in having a faster nail growth rate.
- Osteoarthritis is the most common type of arthritis, affecting an estimated 20.7 million adults in the United States.
- The average American walks 5,900 steps a day. The recommended daily number of steps is 10,000, which is approximately five miles.
- Cigarette smoking increases the risk of peripheral arterial disease (PAD) by several folds and is one of the most prominent risk factors. PAD is a disease in which plaque builds up in the arteries that carry blood to your head, organs, and limbs and usually affects the arteries in the legs, leading to pain and numbness in the lower extremities. In severe cases, PAD may cause infection, gangrene, and lead to leg amputation.
- When our feet are misaligned, the effects can be felt in the muscles in the rest of the body, potentially causing joint pain or even serious injuries. There are two types of foot misalignment: overpronation and excessive supination. Over 75% of the population suffers from foot misalignment.
- Ankle sprains are one of the most common injuries in sports. Because the inner ankle is more stable than the outer ankle, the foot is likely to turn inward from a fall (ankle inversion) which results in an ankle sprain.
- More than one-third of women in America have bunions, a common foot deformity in which the joint that connects the big toe to the foot gets larger and juts out.
- Both Michelangelo’s David and the Statue of Liberty have Morton’s toes. It’s is a foot condition in which the second toe is longer than the big toe. It is also called Greek foot because the ancient Greeks found it aesthetically appealing and incorporated it into paintings and sculptures.
- The feet can contract an array of nasty diseases from communal showers: Plantar warts, athlete’s foot, and ring worm are just some!
And the answer to the trivia question is walking. Walking contributes to your general well-being and improves circulation and weight control.
Remember to look after you feet. If you’re worried you may have foot health issues, get in contact with Dr. Vikki and Dr. Connie today.
If you’re fortunate enough to have all of your limbs, then chances are you take them for granted. Prosthetic limbs, such as feet, are incredibly valuable to amputees because a prosthetic can help restore some of the capabilities lost with an amputated limb. Although prosthetic limbs have still not advanced to the point where they can rival the functionality provided by biological limbs, the capabilities they do provide can be significant.
Here’s a quick look at how prosthetics work to make life easier for amputees.
How Prosthetics Work
While new materials and technologies have modernized prosthetics over the past century, the basic components of prosthetic limbs remain the same. The basic components include:
- The pylon—the internal frame of skeleton of the prosthetic. The pylon provides structural support and has traditionally been formed of metal rods. However, modern technology has allowed for lighter carbon-fiber composites to be used in place of the metal rods. The pylons are sometimes enclosed by a cover (usually made from a foam-like material). The cover can be shaped and colored to match your skin tone in order to give the prosthetic a more lifelike appearance.
- The socket—the portion of the prosthetic device that interfaces with the patient’s limb, stump, or residual limb. Since the socket transmits force from the prosthetic to the body, it must be meticulously fitted to the residual limb to ensure that it doesn’t cause irritation or damage to the skin or underlying tissues. A soft liner tends to be used in the interior of the socket, and a patient may also wear one or more prosthetic socks to achieve a snugger fit.
- The suspension system—this is what keeps the prosthetic attached to the body. The suspension mechanism can come in several forms (straps, belts, or sleeves), although the most common type of suspension mechanism relies on suction.
Even though most prosthetic limbs have these basic components in some form or another, each device is unique and designed for a specific type and level of amputation.
Choosing the Right Prosthetic Foot
Today, amputees have a wide variety of prosthetic feet to choose from, designed for walking, cycling, golfing, swimming, snow skiing, and running. Heavier wood and steel materials have been replaced by lightweight plastics, aerospace alloys, and carbon-fiber composites. But how do you choose the right one for your lifestyle?
There are a number of key factors that you should consider, including materials, comfort, function, energy storage, and multi-axial motion.
- Materials—the materials in a prosthetic foot differ by activity level. Wood, plastic, and foam are usually found in feet designed for people with low activity levels and for those who require stability. Carbon feet meet the functional needs for shock absorption and energy efficiency, and are also lightweight.
- Comfort—a prosthetic foot has to feel good for you to meet your activity goals. Comfort allows you to be more active, and the function of your prosthetic foot directly affects comfort.
- Function—prosthetic feet are designed to mimic the human foot at a specific activity level. For people who can’t walk, the function is largely cosmetic. For those who are most active, a prosthetic foot must mimic a normal foot during the act of walking. It must act as a shock absorber when your heel hits the ground, adapt to uneven terrain, provide a smooth rollover from heel to toe, and provide a rigid lever for propelling forward when you finish your step.
- Energy storage—a foot made with carbon fiber for energy storage gives you a spring in your step as the carbon fiber acts as a spring, compressing as you apply weight and propelling you forward as your foot rolls, returning energy to your step as the spring releases. Some prosthetics have one spring in the heel and a second spring in the forefoot (just what you need for walking in various speeds, running, climbing hills, or descending stairs with a secure, confident stride). With carbon fiber, the longer the spring, the more energy it can store and the more responsive the foot will be.
- Multi-axial motion—some prosthetic feet are designed to mimic the ankle, which allows the foot to move in multiple planes. Multi-axial capability in a foot allows you to raise and lower the forefoot, move the forefoot to the left and right, and roll the foot slightly to the inside or to the outside. Multi-axial motion is needed to walk comfortably and confidently on uneven ground, when your foot must adapt to whatever it encounters.
The Bionic Foot
While prosthetics are the norm for amputees at the moment, the future seems to be leading us in the direction of bionic feet. Bionic feet that can be controlled by the patient’s mind, using sensors implanted inside the muscle tissue, have been proven to work in human-testing trials.
The tiny implanted myoelectric sensors (IMES), which are surgically implanted in the residual muscle tissue about the leg, wirelessly transmit a signal to the foot, telling it to perform a specific action. While this is a breakthrough in prosthetic technology, there are still a few bugs to work out before this becomes a more mainstream option for amputees.
Schedule an Appointment
If you have any questions or concerns about foot health or need guidance in the event you’re in need of a prosthetic foot, do not hesitate to contact the caring and professional team at the Superior Foot and Ankle Care Center.
Massage therapy has long been lauded as an effective treatment for relieving muscle tension, pain, and stress, but research suggests that the scope of its health benefits go much further. While there are different schools of massage therapy, from Swedish massage to shiatsu, all schools involve applying various levels and techniques of pressure to the muscles in order to promote relaxation. When performed by a trained professional, massage therapy can help resolve muscle damage and even prevent injury.
Foot massage is especially important, as the feet are among the most overused and under-cared for parts of the body. Foot massage techniques are deeply rooted in the study and traditions of reflexology, an alternative medicine discipline that focuses on stimulating pressure points in the feet which correspond to specific systems in the body.
The proven stress reduction stemming from reflexology techniques is then extended to alleviating the symptoms of various ailments and conditions. While a foot massage in itself may not be a cure-all, its stress-relieving and muscle-soothing benefits have far-reaching positive effects on your health, from improved circulation to better sleep.
Here is a look at a few reasons why you should schedule a foot massage regimen:
Stress Relief
The strength of massage therapy as a treatment lies in the healing power of the human touch.Massage reduces the levels of cortisol in the body, the hormone responsible for the negative impact of stress. Moreover, massage has also been shown to improve the levels of serotonin and dopamine which are central to depression. Studies have also found massage to be correlated with increased levels of oxytocin, the hormone intrinsic to emotional bonding.
Thus massage not only relieves the physical tension associated with stress, but the sensation of repeated human touch given in a safe environment produces positive emotions proven to improve symptoms of depression and anxiety. But don’t feel restricted to a professional massage therapist: the emotional benefits associated with massage are just as – if not more – accessible when performed by a loved one.
The benefits of this stress release are expansive: massage can be used as an effective treatment for conditions in which depression and anxiety are the primary symptoms, for example the hormonal changes experienced during PMS and menopause. For this reason, massage has also proven useful in treating migraines and headaches caused by chronic stress. While massage isn’t intended to replace medication for a condition in which depression is a symptom, it is an extremely effective therapy to supplement medical treatment.
Improved Circulation
A 10-20 minute foot massage before bed can work wonders in improving your blood circulation. The kneading pressure applied during a massage helps to improve blood flow through congested areas, allowing fresh blood to flow in. The motions of squeezing and pulling work to clear the muscles of lactic acid, while improving lymph circulation to clear your system of metabolic waste. Better circulation improves blood flow, lowers blood pressure, and enhances overall body function. This is especially helpful for diabetic patients, who struggle with poor circulation in their lower extremities.
Relieves Pain While Reducing Injury
Just 10 minutes of massage following a workout can help reduce inflammation, allowing your body to recover more effectively. Combining strengthening exercises, stretching, and regular foot massages not only facilitates the recovery of existing foot injuries, but helps prevent new injuries from occurring.
Moreover, regular foot massage with deep pressure applied to the arch can alleviate the pain associated with any deformity or weaknesses in the foot, such as with flat feet and plantar fasciitis.
Better Sleep
Due to its expansive stress relieving benefits, foot massage has also been shown to enable relaxation and improve sleep in patients who find it difficult to rest otherwise. This includes individuals who are under chronic stress or struggle with insomnia. Massage therapy has even been shown to improve the rest of patients undergoing chemotherapy. New parents will also be pleased to find that basic massage techniques can even work on newborns, coaxing finicky infants to sleep.
Schedule a Consultation with Dr. Vikki and Dr. Connie
Don’t wait until your foot health is compromised to take advantage of the benefits foot massage has to offer. Schedule a consultation with trusted podiatrists Dr. Vikki and Dr. Connie at the Superior Foot & Ankle Care Center to learn more today.
Despite the way our species evolved away from climbing trees to walking on flat ground, some people are still walking around with monkey-like feet. In fact, you may be surprised to learn that about eight percent of the population, or 1 in 13 humans, may have a midtarsal break in their foot characteristic of non-human primates. These are also referred to as prehensile feet.
What is a Midtarsal Break?
The midtarsal break is a medial shift in the center of the pressure trajectory with dorsiflexion of the midtarsal joint (the joint between the talus and the navicular bone as well as the joint between the calcaneus and the cuboid bone), occurring during the gait of an unstable foot, when the body transfers weight from rearfoot to forefoot.
A midtarsal break, also known as floppy feet, tend to occur in people with flatter feet and higher body mass indexes than people with stiffer feet. They also tend to roll their feet more, causing a motion called hyperpronation (they land on the outside of their feet and roll dramatically inward). This allows for the foot to relax its joints and ligaments, creating a midtarsal break.
What are Prehensile Feet?
Prehensile feet are lower limbs that possess prehensility (the ability to grasp like a hand). They are most commonly observed in monkeys. Due to the development of bipedalism in humans, the hands became the focus of prehensility and the feet adjusted to more of a stabilizing role. It may be possible, however, that the foot does not reach its limits of dexterity due to the constant muscle tension needed in stabilizing and balancing the foot to hold up the legs and the rest of the frame.
People with prehensile feet can grasp small objects between their toes, manipulating them as with a hand with the ankle functioning like the wrist. As toes are much shorter than fingers, and since the ball of the foot is so large and obtrusive, grasping does not function as in a normal hand and the foot is not able to hold very large or heavy objects.
Chimpanzee Feet vs. Human Feet
Conventional wisdom has always claimed that the human mid-foot is rigid, which allows for more efficient walking while chimpanzees and other apes have flexible feet better suited to grasping branches as they move through the trees.
Human feet are both rigid and pliable depending on the need. The human foot is a spring arch that should be able to drop and lift with every step. Human legs angle in from the hip to the knee, allowing our feet to fall directly under the pelvis and our pelvic muscles are much stronger, as well, allowing for a stable upright environment.
Chimpanzees are often referred to as knuckle-walkers because they only walk on two legs for short distances due to the differences of our legs and spine. Chimpanzees can’t straighten their legs like humans and they don’t have a lumbar curve, which makes weight bearing and walking more difficult. Chimpanzee legs are also set wide apart and weak pelvic muscles force their whole body to transfer weight from side to side during each step.
Yet, while chimp feet and bodies can’t do what humans can, it doesn’t appear to be a problem if our feet work like chimpanzee feet. In fact, two studies (one from Boston University and the other from Dartmouth) have proven that about eight percent of the population have the mobility of chimpanzee feet, which allows some societies to functionally adapt their feet and calf muscles to allow them to climb trees like chimps do.
While eight percent of the population exhibits a flexible midtarsal break in their feet, people with midtarsal break rarely realize that they have one, as it doesn’t affect their gait.
The Walking Test
So how do you know if your feet might have a midtarsal break? Take a stroll on sand. Here are a couple of tips:
- If you have high arches, you probably have stiff muscles and ligaments, which means that you don’t have a midtarsal break.
- If you have a midtarsal break, the fold in your foot will pinch the sand upward. Look for a small ridge in the upper-mid portion of your footprint.
Talk to Dr. Vikki and Dr. Connie
If you have any questions or concerns about whether or not you have prehensile feet with a midtarsal break, and if there are any unique factors you have to account for regarding your foot health, feel free to book an appointment with Dr. Vikki and Dr. Connie today.
Skin on the feet or ankles can discolor for any number of reasons, ranging from staining from wet clothes or boots to serious medical conditions. Yet, if the discoloration isn’t immediately explainable by simple environmental factors, then it’s in your best interest to seek medical attention.
Here are some things that you should know about some of the more serious problems that could be causing your feet discoloration.
Venous Insufficiency
Venous insufficiency, also known as chronic venous insufficiency or chronic venous stasis, is a problem with the flow of blood from the veins of the legs back to the heart. This occurs when the valves in the veins of the leg don’t work properly, causing fluid pools to form, which can lead to other problems including varicose veins.
Venous insufficiency can be caused by blood clots, deep vein thrombosis, or high blood pressure inside the leg veins. You are more likely to have venous insufficiency if you:
- Are older
- Are female
- Are overweight
- Don’t get enough exercise and tend to lead a sedentary lifestyle
- Smoke
- Have a family history of varicose veins
Symptoms may include:
- Swelling, often in the ankles
- Varicose veins
- Itching
- Cramping
- General weakness
- Skin sores (ulcers)
- Aching or a feeling of heaviness
- Changes in skin color/feet discoloration
- Thickening of the skin on your legs or ankles
In order to treat venous insufficiency, your doctor may ask you to:
- Wear compression stockings
- Get more exercise (especially walking)
- Avoid standing or sitting for long periods of time
- Keep your legs elevated when lying down
In more severe cases, you may have to undergo surgery to correct venous insufficiency. Your doctor may suggest one of the following types of surgery:
- Surgical repair of veins or valves
- Removing (stripping) the damaged vein
- Minimally invasive endoscopic surgery—the surgeon inserts a thin tube with a camera on it to help see and tie off varicose veins
- Vein bypass—a healthy vein is transplanted from somewhere else in your body (this procedure is generally used when the upper thigh is affected and only for very severe cases after nothing else has worked)
- Laser surgery—uses lasers to either fade or close the damaged vein(s) with strong surges of light in a small, specific place. It involves no surgical cuts.
Rocky Mountain Spotted Fever
Rocky Mountain spotted fever is a bacterial infection transmitted by a tick. Without prompt treatment, Rocky Mountain spotted fever can cause serious damage to internal organs, such as your kidneys and heart.
Although many people become ill within the first week after infection, signs and symptoms may not appear for up to 14 days. Symptoms can include:
- High fever
- Chills
- Severe headache
- Muscle aches
- Nausea and vomiting
- Restlessness and insomnia
- Rash—the red, non-itchy rash typically appears a few days after the initial signs and symptoms begin. It first appears on your wrists and ankles, and can spread in both directions.
People who develop Rocky Mountain spotted fever are much more likely to avoid complications if treated within five days of developing symptoms.
Ankle Sprain
An ankle sprain is an injury to the tough bands of tissue (ligaments) that surround and connect the bones of the leg to the foot. The injury typically occurs when you accidentally twist or turn your ankle in an awkward way. This can stretch or tear the ligaments that hold your ankle bones and joints together.
Symptoms of an ankle sprain can include:
- Swelling
- Bruising
- Pain
- Inability to put weight on the affected ankle
- Skin discoloration – primarily ankle and foot discoloration
- Stiffness
Treating a sprained ankle is important to promote recovery and to prevent further discomfort. If your sprain is mild, you should be able to treat it at home by:
- Using elastic bandages to wrap your ankle
- Wearing a brace to support your ankle
- Using crutches
- Elevating your foot with pillows while resting or sleeping to help reduce swelling
- Taking ibuprofen (Advil) or acetaminophen (Tylenol) to manage swelling and pain
- Getting plenty of rest and not putting weight on your ankle
- Applying ice every 20-30 minutes, three to four times per day
Surgery for ankle sprains is rare, but it may be performed when the damage to the ligaments is severe or when the injury doesn’t improve with non-surgical treatment. Surgical options include:
- Arthroscopy—your doctor will look inside the joint to see if there are any loose fragments of bone or cartilage
- Reconstruction—you doctor will repair the torn ligament with stitches. They may also use other ligaments or tendons around the foot or ankle to repair the damaged ligaments.
Proper Diagnosis
If you’re experiencing any feet discoloration, and the cause is not immediately known to you, you should seek out medical attention. A proper diagnosis can go a long way to helping you treat and quickly recover from whatever is causing your foot discoloration.
If you have any questions or concerns about feet discoloration, book an appointment with Dr. Vikki and Dr. Connie, so that they can help you get the right answers and treatment.
More...
You may have heard one of the many myths surrounding broken toes: that it will heal on its own, or that it’s okay as long as you can still walk on it. While reassuring, these common misconceptions are entirely false, and can have potentially severe consequences. Leaving a broken toe untreated can result in various complications, from misaligned bones and infection to arthritis and permanent foot pain. The thought of a doctor visit or hospital bill may make you cringe at first, but your feet will thank you for it in the long run.
Here is a look at the signs that your toe is broken, the dangers of avoiding treatment, and the steps you need to take to make sure your toe heals properly.
Signs Your Toe Is Broken
Even the smallest of accidents can result in toe trauma: dropping an object on the foot or stubbing your toe are common misfortunes that often lead to injury. Moreover, repetitive trauma to the toe over time can result in a stress fracture. While it’s tempting to try to tough it out, it’s important to listen to your pain to identify whether or not your toe is fractured.
It usually requires significant force to break a bone, although a little less so for the toes since their bones are so small. Regardless, the instance of fracture will be extremely painful. The toe will begin to swell as the fractured bone bleeds, resulting in bruising as the blood reaches the skin. You may also see blood pool beneath the toenail. In many cases an injury to the toe also involves damage to the toenail, which further increases your risk of infection should the toenail expose the tissue underneath. The fracture usually makes it extremely painful to walk, although this is not always the case. Even if you can still manage to walk on the toe, that doesn’t eliminate the possibility of a fracture.
Seek prompt medical attention if your toe shows signs of:
- Swelling
- Pain
- Bruising, or blue or gray spots surrounding the site of trauma
- Stiffness
- Trouble Walking
- Deformity
- Infection
- Bleeding, especially beneath the toenail
- Coldness, numbness, or a tingling sensation indicative of nerve damage
Complications of an Untreated Broken Toe
Leaving a broken toe untreated can have serious and long term complications, including, but not limited to:
- Infection: If the injury has left an open wound, or especially if there is damage to the toenail, you are at risk of contracting an infection. Any exposure of a broken bone can lead to a bone infection (osteomyelitis), which is usually caused by the bacteria staphylococcus aureus. Once diagnosed, your doctor may implement antibiotics straight into the bloodstream intravenously, or you may need to take medication for up to six weeks. If the infection is severe, your doctor may have to perform surgery to remove the infected bone.
- Compound fracture: A compound fracture is when a broken bone penetrates the skin, leaving the bone vulnerable to infection.
- Deformity: An untreated broken toe has a high likelihood of healing incompletely or improperly, potentially resulting in crookedness or deformity which may require corrective surgery down the road.
- Osteoarthritis: An improperly healed fracture can lead to a future of osteoarthritis as you age, generalized foot pain and discomfort, as well as an increased likelihood of further foot injury.
Toe Fracture Diagnosis and Treatment
Your podiatrist will order an X-ray to confirm a toe fracture. Once properly diagnosed, a mild toe fracture can be treated at home under the guidance of your trusted podiatrist. Home treatment essentials include elevating the foot above the level of the heart in order to decrease swelling, icing the injury for 20 minutes every 2 hours for the first 2 days, and of course rest and crutches to avoid bearing weight on the injury while you recover. OTC acetaminophen or ibuprofen should be sufficient for coping with the pain, although your doctor may prescribe a stronger medication if your fracture is severe.
If the fracture is minor or located in one of the small toes, your doctor may simply implement buddy taping, which involves taping the damaged toe to its neighbor for support while it heals. In cases where the toe fracture becomes rotated or displaced, the doctor will need to perform a reduction. This involves administering a shot of local anesthesia before realigning the toe back into its proper position.
Casting may be required in more severe fractures: where the big toe is injured, the joint is damaged, the injury involves various small toe fractures at once, or if a bone in the foot is injured in addition to the fractured toe. When wearing a cast, a sturdy shoe should be worn to provide maximum comfort and support. If all goes well, the fracture should take up to six weeks to heal.
Schedule a Consultation with Dr. Vikki and Dr. Connie
If you have suffered injury to your feet, toes, or ankles, don’t wait for complications to arise.Schedule a consultation with trusted podiatrists Dr. Vikki and Dr. Connie at the Superior Foot & Ankle Care Center today.
Whether you’re trying to help out a friend or you’ve hurt your own foot, knowing how to properly deal with and take care of an injured foot can save you a lot of stress and problems later.
Here’s a quick how-to guide on how to properly take care of and bandage an injured foot or ankle.
How to Stop Any Bleeding
If there is any blood involved, it is important to first wash your hands and put on medical gloves (if available) before applying direct pressure to the wound. If gloves aren’t available, use many layers of clean cloth, plastic bags, or the cleanest fabric available between your hands and the wound.
In order to stop the bleeding, you should:
- Have the injured person lie down and elevate their foot for a full 15 minutes
- Remove any visible objects in the wound that are easy to remove
- Remove clothing and jewelry from the general area of the wound in case of swelling
- If blood soaks through the cloth, apply a clean one
How to Wrap an Injured Foot or Ankle
To prevent further injury and encourage proper healing, you should make sure that you protect and compress your foot, as well as rest, ice, and elevate your injury. There are a couple different types of material that you can use to wrap and compress an injured foot or ankle, including an elastic cloth bandage and athletic tape.
Wrapping with an Elastic Cloth Bandage
- Begin wrapping—place the end of the bandage where the toes meet the foot. Begin by wrapping the bandage around the ball of the foot. Hold the end of the bandage against the ball of the foot with one hand, and use the other to bring the tail around the foot from the outside. Make sure to keep the bandage tight, but not so tight that it decreases blood flow to the foot and toes.
- Work your way toward the ankle—wrap the ball of the foot twice, to hold the bandage in place, then begin moving up towards the ankle, being sure to leave at least one-half inch of bandage overlapping the previous layer. Make sure the layers are smooth and even with no unnecessary bulges or lumps. Start over if you need to do the job more neatly.
- Wrap the ankle—when you get to the ankle, bring the end of the bandage up outside of the foot, over the instep and around the inside of the ankle. Then bring it around the heel, back up over the instep, under the foot and around the ankle. Continue making a figure eight around the ankle several times to fully stabilize the ankle.
- Finish the wrap—the last wrap should rise several inches above the ankle to help stabilize it. Use the metal fasteners or medical tape to secure the remaining bandage. Excess bandage can also be tucked under the last layer, provided there’s not too much excess.
Wrapping with Athletic Tape
- Decide if athletic tape is right for you—while athletic tape works to wrap an injured ankle, it is primarily made to wrap an uninjured joint before physical activities to avoid injury, not to protect an already injured ankle.
- Begin with an underwrap—underwrap is a non-adhesive material used to wrap the foot and ankle before tape is applied, so that the tape doesn’t pull at the surface of the skin. Starting at the ball of the foot, wind the underwrap around the foot up to the ankle, leaving the heel uncovered.
- Secure the anchor—cut the strip of tape long enough to wrap one and a half times around your ankle. Wind it around your ankle, over the underwrap, to hold the underwrap in place.
- Create a stirrup—place the end of a piece of tape on one side of the anchor. Bring it down under the arch of the foot and back up to the other side of the anchor. Press it lightly to secure it in place. Repeat with two more pieces of tape overlapping the first one to create a sturdy stirrup.
- Create an X over the foot—place the end of a piece of tape at the ankle bone and run it diagonally over the top of the foot. Bring it down under the arch and toward the inside of the heel. Then bring it around the back of the heel and back up over the foot to create the other part of the X.
- Make a figure eight—place the end of a piece of tape on the outside of the ankle, just above the bone. Run it over the top of the foot at an angle, then bring it under the arch and up the other side of the foot. Next bring it around the ankle and back to the point where you started. Use another piece of tape to make a second figure eight that overlaps the first one. This will ensure that the wrap is held securely in place an provides enough support for the ankle to heal properly.
If a foot or ankle injury is serious and/or life-threatening, it’s important to call an ambulance. However, if the pain is manageable and you need help in dealing with the injury and getting back on your feet as soon as possible, be sure to get in contact with Dr. Vikki and Dr. Connie today.
Itchy feet can become the bane of any day: you’re either driven mad trying to resist the urge to scratch; or by the redness, swelling, cracking, and flaking as a result of uncontrollable itching. While the cause could be something benign such as dry skin or excessive sweating, it could also indicate an infection or undiagnosed skin condition. Moreover, if left untreated, other complications could arise, such as a secondary infection.
The itching and burning will only continue to plague you until you accurately identify the source and treat it accordingly. Besides the obvious bug bites or allergic irritation, itchy feet are most commonly caused by a fungal infection or an underlying skin condition. In rare cases, itching could also suggest the presence of another medical condition, such as diabetes. Only examination from a trusted podiatrist can accurately diagnose your foot condition.
Here’s a look at the possible causes of itchy feet, treatment, and prevention tips to keep your feet feeling fresh.
Fungal Infection
When itchy feet are the main symptom, fungal infection is usually the primary suspect: specifically, tinea pedis, or athlete’s foot. Constant exposure to sweat and bacteria, in addition to walking barefoot on contaminated surfaces, make your feet the ideal breeding ground for fungal infection.
Athlete’s foot is an extremely contagious fungal infection which is easily spread through contact with infected surfaces, usually in damp spaces such as showers and gym locker rooms. In fact, it can even be spread through shared towels or linens. The first sign of infection is a dry, scaly rash that causes unbearable itching on the bottoms of the feet and between the toes. While the symptoms can be abated by certain over-the-counter creams, only a podiatrist can effectively cure you of the infection. Once cured, vigilant prevention should be practiced to avoid re-infection.
Skin Conditions
A number of skin conditions can lead to insatiable itching of the feet.
Eczema: Eczema can affect most parts of the body, but dyshidrotic eczema specifically affects the feet and hands. It is characterized by tiny itchy blisters formed on the soles of the feet, which then dry and cause cracking on the skin. If not properly cared for, the exposed skin can become vulnerable to infection. Since dyshidrotic eczema can share symptoms with other skin conditions, a skin sample will likely be taken for proper diagnosis.
Contact dermatitis: Contact dermatitis is a skin irritation that results from contact with an allergen or irritant, which appears similar to a rash. Allergic contact dermatitis is caused by skin exposure to an allergen, triggering an allergic reaction in the affected area. Irritant contact dermatitis is distinct in that it does not involve the immune system, but is instead the result of skin damage caused by exposure to an irritant that rids your skin of its protective surface oils. Common triggers of contact dermatitis include poison ivy, latex, nickel, chemical fragrances, topical medications, and leather.
Psoriasis: Psoriasis is an autoimmune disorder which causes rapid skin cell turnover, resulting in incredibly itchy and scaly dry patches called plaques. The plaques are the result of layers of new skin cells rising so quickly that the dead skin piles atop the surface, rather than gradually sloughing off, form dry patches of thickened skin. Plaques are commonly found on the bottoms of the feet, as well as the elbows and knees.
Additional Sources of Itchy Feet
Here are a few potential, albeit less likely, perpetrators of itchy feet:
- Diabetes: Skin conditions can sometimes indicate diabetes. A condition called eruptive xanthomatosis produces small itchy bumps on the skin as a result of severe diabetes. The condition subsides once the diabetes is managed and under control.
- Scabies: Scabies is an infection of the human itch mite which burrows just below the skin to lay its eggs. The infestation causes intense itching which worsens at night, a pimply rash, and tiny blisters. You can also see traces of the burrows on the skin, which appear as thin whitish lines along the surface. Scabies is easily spread, and should receive medical attention to stem the infection right away.
- Pitted Keratolysis: Pitted keratolysis is a non-contagious bacterial infection, caused by wearing damp, restrictive footwear. It produces shallow pits beneath the toes and soles of the feet, accompanied by itching, burning, and an extremely foul odor.
Prevention Tips
The feet are constantly plagued by bacteria, and need to be cleaned just like your hands. To keep your feet comfortable and fresh, follow these basic hygiene tips:
- Avoid walking barefoot anywhere, especially on damp communal surfaces.
- Always wear dry, clean socks and shoes made of breathable materials.
- Wash your feet thoroughly, and do your best to keep them dry.
- If someone you know has an infection, do not share towels or linens, and protect your feet from contaminated surfaces.
- Keep your toenails trimmed and clean.
If you suspect an infection is already present, schedule an examination with a reputable podiatrist right away.
Schedule a Consultation with Dr. Vikki and Dr. Connie
If itchy feet are wreaking havoc on your life, schedule a consultation with esteemed podiatrists Dr. Vikki and Dr. Connie at the Superior Foot & Ankle Care Center today.
There are some professions out there that cause a lot of stress to the arches, balls and heels of the feet, which can lead to other spinal and back discomfort issues, fatigue, and various mental health problems. Health care professionals, construction, hairdressing, office jobs, as well as landscaping jobs are all very different professions with this commonality—all are very stressful for the feet and can cause foot problems and pain.
Health Care Professionals
Hospitals are one of the busiest public places where employees work long hours. Nurses and doctors are always on the move during their long shifts, walking miles each day to serve and assist their patients. This can lead to numerous foot problems such as bunions, flat feet, ingrown nails, and heel spurs.
The foot has dozens of bones, joints, muscles, nerves, blood vessels, tendons, and layers of connective tissue. When working in the health care profession and working those long hours on your feet, the body tissues in your feet can become very stressed, achy, and swollen. If there is prolonged inflammation, this will actually form scar tissue and tire out the bones of the feet.
For those that work in the healthcare profession, be sure to wear comfortable, arch-supportive shoes with shock-absorbing soles, and get them fitted by a professional to make sure they are exactly right for your feet.
Construction Workers
Construction work is a heavy-duty, active profession that puts a lot of strain on the entire body, including the feet. Construction workers have to work in very challenging weather and circumstances and are on their feet for their entire day besides some small breaks. They are required to bend and lift and tend to end their shifts very exhausted and, sometimes, in pain.
The most common injury experienced by construction workers are ankle and foot injuries. Construction workers often develop flat feet or severely painful arch problems that can hinder their performance and their lifestyle outside of work.
Construction workers should invest in good footwear, such as steel-toe boots, that are a high quality brand able to prevent blisters, calluses, and protect the feet from anything heavy that could fall on them. Weeks before working in new boots, it’s key to break them in as much as possible.
If construction workers experience a foot injury, they should take days off to recover and see a medical professional like a podiatrist who can identify the problem and prevent further pain and injury.
A great tip is to freeze a bottle of water before heading out to work. When you get home, roll your feet over the frozen bottle. Not only will this exercise reduce inflammation and pain, but also the motion of the rolling will get the blood moving in your feet.
Hairdressing
Hairdressers often complain of foot pain at work, and this can result from repetitive straining motions; but also from a lack of supporting your feet and preventing foot problems well before pain and problems occur. If you are a hairdresser, try to remember to not lean on one dominant side when cutting hair.
Try to ground yourself and distribute your weight evenly on both of your feet. This will prevent pinched nerves and developing uneven arches.
Another way to prevent foot problems is to exercise and have a balanced diet. The more weight you carry, the more strain that’s placed on your feet, legs, and back. It’s simple—the more you weigh, the harder it is for you to be standing on your feet day all day.
Invest in a rubber mat for your chair and work space area. This will prevent developing foot problems and will keep your back healthy, too. Wear good shoes with less than a 1.5-inch heel to avoid severe heel pain. Absorbent pads and laces on the body of the shoe can help provide optimal support. Consider orthotics if you’re already experiencing foot pain as this will alleviate and correct current problems.
Preventing Foot Problems
Healthy feet are the key to a healthy life. Talk to a podiatrist professional such as the great team at the Superior Foot and Ankle Care Center and learn more about what you can do to keep your feet healthy.